What is the operation for urinary incontinence. Where is TVT-o carried out. Laser lifting of the vaginal mucosa for urinary incontinence
Is surgery always necessary for urinary incontinence in women? Urinary incontinence is clinical manifestation pathological process in humans, which can affect women and men. As a rule, this condition is observed in patients whose age is over forty years. But it is in women this manifestation occurs much more often, which creates problems in life. If there is urinary incontinence in women, surgery in most cases is a necessary measure.
Urogynecology and urodynamics: theory and practice. 4th ed. Evaluation of various surgical procedures. female stress urinary incontinence Clinical guidelines Batch report on the surgical treatment of female stress urinary incontinence. American Urological Association.
Surgical treatment of stress incontinence. Practical urogynecology. 1st ed. Vaginal screed: four years later. To view latest version this review on English language. Urinary incontinence is the most common form of incontinence in women and reduces their quality of life. Women with stress urinary incontinence may also have problems having sex because urine leakage may occur. One in three women over the age of 18 will experience stress urinary incontinence at some point.
- Availability definitions chronic pathologies and history taking. Urination is strongly influenced diabetes, urolithiasis disease, adenoma operations, postponed childbirth.
- A study of the vagina, which allows you to determine the presence of scars, the condition of the urethra, bladder, and also to identify the presence of uterine prolapse.
- An ultrasound of the pelvis, which gives an idea of how much urine is left immediately after the urination process.
- Urodynamic study. AT this case the help of the patient will be required, who must keep a diary, where to record the amount of fluid drunk, the amount of urine excreted and how often urination occurs.
This condition can be caused by:Enuresis occurs due to muscle weakness or after a change in the angle of attachment of the urethra.
Surgery to treat this problem has become less invasive over the years, and there are several various kinds Operations: Middle urethral sling operations are commonly used to treat urinary incontinence. women who have undergone their first incontinence prevention surgery, as well as women who have failed in a previous operation. During middle urethral sling surgery, a band is placed under the urethra, the pipeline carries urine to the bladder. With force, such as coughing, the band compresses this tube, thereby providing necessary support to prevent leakage of urine.
- tribal activity;
- surgical intervention;
- hormonal changes;
- injuries that have been rendered to the bladder.
Indications for surgery for urinary incontinence are:![]()
There are two main ways to do this by inserting the tape behind pubic bone through the abdomen or through the groin. We investigated the effects of operations from the middle of the urethral sling using these two different methods implementation. We also compared various ways strip insertion, as well as the use of strips from different materials. The purpose of this review was to determine the effectiveness of these surgeries in the treatment of stress urinary incontinence and to help determine the level of complications or potential problems.
Main results of the review. We have conducted a thorough search medical literature until June. These trials have shown that more than 80% of women with stress incontinence are cured or have significant improvement in symptoms, both types of surgery, up to five years after surgery. We found this to be true regardless of the lane used and the insertion route, because the studies used different quality-of-life questionnaires, we could not pool our results for analysis.
- Weakness muscle tone pelvic floor because of stressful situation. If the situation is not so neglected, then a set of exercises and medication is prescribed. But the effectiveness of such treatment is insignificant, for this reason, either surgery is prescribed, or the installation of a special pessary.
- Special health conditions that increase the risk of incontinence. These include: diabetes, intense exercise and obesity.
In the male half of humanity, urinary incontinence often occurs after surgery to remove the prostate gland.
However, the available quality of life information shows that it improves as a result of these surgeries, although there is no obvious difference between the two procedures. Only a few studies have provided information on the effectiveness of test strips more than five years after surgery, and the evidence we have been able to assess suggests that positive effects are saved.
Strips that run behind the pubic bone appear to have a greater risk of bladder injury during surgery and problems emptying the bladder completely after surgery. However, this surgery causes less pain in the groin in the short term. Some limited evidence suggests that this method of inserting the strip has a lower risk of repeat surgery in long term that strips inserted through the groin. Moderate-quality evidence suggests that the reported rates of complications associated with the strips are usually low, eg, vaginal strip erosion in about 2% of cases for both routes of insertion of the strips.
Types of surgery
The nature of the intervention in different sexes can differ significantly, but still there are general methods applied without regard to gender. These include sphincter implantation or sling surgery for urinary incontinence.
The rest of the operations are applicable exclusively for women, since during their implementation the reproductive organs are used to fix the urethra.
The reported incidence of problems, including pain during intercourse, was low, and leakage of urine during intercourse was improved after the introduction of these strips. Most of our results are based on moderate quality evidence. Most trials do not contain clear descriptions of their methods, leading to some degree of uncertainty about the results. At present, only a limited number of randomized controlled trials publish data beyond five years after surgery, data on the efficacy and safety of these long-term procedures lag far behind short- and medium-term data.
Sling surgery is indicated in cases where there is stress urinary incontinence of the second and third degree, but only in the presence of weakness of the internal sphincter or in the case of a hypermobile urethra. This procedure consists in maintaining the urethra by suspending it with a prosthesis.
During surgery, you will need a prolene loop or sling, which consists of the tissues of the patient himself or a donor. The latter option involves the excision of a tissue flap from two to ten centimeters. A sling made from donor tissue must be prepared in advance and kept in a special solution.
We encourage researchers to publish data over longer follow-up periods to improve the reliability of long-term results in this area. Middle urethral slings are the most widely studied surgery stress urinary incontinence in women and have good profile safety, regardless of the route, they are very effective in the short to medium term Ultimately, there is growing evidence that, with the exception of groin pain, fewer side effects using the transbutant approach.
The most popular as a sling are synthetic nets that do not cause allergic reactions. It is the mesh that is best tolerated by patients, which allows for surgical intervention without looking for a donor.
As for slings for men, they are somewhat different from those for women. Slings must be easily adjustable and in no case overtighten the urethra.
When comparing transbutant methods with medial and lateral insertion versus lateral to medial insertion, there is no evidence to support the use of one of these approaches over the other. However, for retropubic bands ascending path was more efficient than the downward path.
A good example illustrated in this review is the need to report long-term outcome data from many existing trials. This will greatly increase the body of evidence and clarify the uncertainty about long-term effectiveness and adverse event.
- Women do not need to make strip incisions, since the operation can be performed through the vagina. The specialist in this case excised the vagina and sticks a loop there.
- At strong half humanity, this manipulation is carried out through the scrotum area.
Urinary incontinence is a very common and debilitating problem that affects about 50% of women at some point in their lives. Urinary incontinence is an inherent or predominant cause in 30%-80% of them. Mid-urethral sling surgery involves passing a small strip through the retropubic or obturator space, with entry or exit points in the lower abdomen or groin, respectively. This review does not include individual split strips.
To evaluate the clinical effects of midline urethral sling surgery in the treatment of stress urinary incontinence, urodynamic stress incontinence or mixed urinary incontinence in women. Document search strategy. Collection and analysis of data. The two review authors independently assessed the methodological quality of potentially eligible studies and extracted data from the included studies.
The loop must be fixed with a non-absorbable thread, one end of which is simply sewn to the abdominal muscles. In order to do this correctly, a puncture in the peritoneum is required. As a result, the urethra becomes in limbo, and its walls are well fortified.
The effectiveness of this surgical intervention is quite high, that is, as statistics show, the success of the operation for urinary incontinence in women is from seventy to ninety-five percent.
Fewer studies reported medium- and long-term data, but subjective healing was similar across groups. The reverse path from bottom to top was more efficient than upper way down for subjective healing. This resulted in a significant reduction in urinary dysfunction, bladder perforation, and vaginal erosion of the bands.
Short-term and medium-term subjective healing rates were similar between inserted transcoturator strips using the medial to lateral and lateral medial approach. Moderate-quality evidence showed that urinary dysfunction was more common in the medial-lateral group, but vaginal perforation was less common with the medial-lateral approach. Due to the very low quality of the evidence, it is unclear whether a lower incidence of vaginal epithelial perforation affects vaginal strip erosion.
Recovery in this case is about two weeks. An interesting fact is that a person is discharged after surgery on the day of manipulation or the next.
Sometimes hospitalization can take several days, and the help of a catheter is required, which greatly facilitates urination. Before the patient fully recovers, he should completely give up driving and physical exertion.
The translations on this site were made possible thanks to the financial contribution of the French Ministry of Social Affairs and Health and public research institutes Canada. Urinary incontinence is defined as any involuntary leakage of urine at the beginning of the gene. There are several types of urinary incontinence.
Urinary incontinence: This results in urgent needs that cannot be saved. Weakness of the perineal muscles responsible for maintaining the bladder and urethra.
- Urinary incontinence: Leaks occur during physical exertion.
- Mixed urinary incontinence: it combines leakage with effort and leakage with power.
- Weak urethral sphincter.
This manipulation is prescribed in the case when there is stress urinary incontinence. Surgery lies in the fact that the tissues of the vagina are hemmed, this leads to the fact that the urethra no longer sags. Anterior plasty can be performed intravaginally or through the peritoneum. The first variation is more physiological, that is, it is much easier to carry.
Her crotch is exposed severe stress during pregnancy and especially childbirth. Finally, the lack of hormones after menopause leads to tissue drying and additional fragility. When pelvic rehabilitation has failed or urinary incontinence is very important, intervention is currently one of the most effective ways permanent elimination of stressful problems.
Currently no active drugs at stress incontinence urine. It consists of positioning a small strip of synthetic material under the urethra. This tape, like a hammock, will remain under the urethra, supporting it during leak prevention efforts. Various strips are available various systems delivery. Your surgeon will choose the one that best suits your case and experience.
But the choice of how to do the operation for urinary incontinence depends on the specialist, who evaluates the history and general state your patient. Access to the required area can be made laparoscopically or through a traditional incision.
The specialist dissects the vaginal mucosa, then separates from the muscles, which are subsequently sutured with non-absorbable sutures. This type of surgical intervention preserves the elasticity of the vaginal walls, which allows you to subsequently give birth normally.
Note that all urinary incontinence is not covered by this procedure. The choice of this method will be made by your doctor after you would have checked you and asked if necessary some exams such as urodynamic evaluation. Diagram of female pelvic anatomy.
Placement of the suburethral strip. Before the procedure: as with any surgical procedure, an anesthetic consultation is carried out a few days before the operation. Choice of anesthesia: local anesthesia, local anesthesia or general anesthesia are carried out by the surgeon and anesthesiologist in accordance with your data and taking into account your opinion.
The recovery period after this operation is about two months, during which it is necessary to carefully monitor hygiene and prevent constipation. The only disadvantage of such an intervention is high probability scar formation.
 Colposuspension is also used to eliminate the causes of enuresis, it is directly related to the use of vaginal ligaments, on which the urethra will subsequently be attached. This manipulation serves as the main operation, which is assigned in the case of high risk that stress urinary incontinence will develop again.
Colposuspension is also used to eliminate the causes of enuresis, it is directly related to the use of vaginal ligaments, on which the urethra will subsequently be attached. This manipulation serves as the main operation, which is assigned in the case of high risk that stress urinary incontinence will develop again.
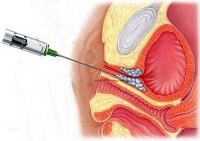
The procedure is performed after a recent urine test confirms that you do not have an infection urinary tract. In the event of an infection, your intervention is delayed until the urine is sterilized. In the operating room, in the gynecological position, three small incisions are made, one of 1.5 cm inside the vagina, two of a few millimeters in the pubis or at the base of the thighs. The strip is skipped and placed under the urethra with the help of needles.
At the end of the procedure, the tube can be placed in the bladder and the swab in the vagina. The duration of the intervention is 20 to 30 minutes. A few hours after consultation with your surgeon, the urinary catheter and a vaginal tampon. The duration of hospitalization usually ranges from a few hours to 48 hours. The procedure is not very painful.
- Anesthesia for the implementation of colposuspension is used only general, since the operation is performed by the band method or laparoscopically. But thanks to this, the recovery period is significantly delayed.
- Before the operation is performed, the patient must lie on her back and spread her legs. Next, the specialist inserts a special catheter with a balloon into her ureter. Surgery involves an incision in the lower abdomen, which can be longitudinal or transverse.
- The balloon is necessary in order to introduce a prepared sterile solution into the bladder, which allows you to better visualize the organ. given area specialists should not touch with a scalpel, since here the muscle membranes must be intact.
- The specialist separates the bladder, and at this time the fingers must be inserted into the vagina and control the process.
- The drainage tube should remain in the wound, and the catheter to facilitate urination in bladder should be five more days. This period the patient must be in bed.
But after laparoscopy in case of urinary incontinence in women, the period bed rest is significantly reduced.
Sometimes patients report problems with urination, which are easily solved with the help of a catheter.
stress urinary incontinence- involuntary release of urine during exertion or physical activity(laughing, coughing, sneezing). Stress urinary incontinence can occur in both young and old. Stress urinary incontinence is most common in postmenopausal women.
Diagnosis and causes of stress urinary incontinence
- Complaints of the patient about leakage of urine during physical exertion, coughing, changing body position
- Inspection in the chair, "cough test". The patient in the chair is asked to cough. In the presence of stress incontinence, involuntary release of urine occurs.
- Ultrasound of the bladder, determination of residual urine. For surgical treatment important condition is the absence of residual urine in the bladder after urination
- Cystoscopy. Performed to exclude vesicovaginal fistulas, which may be the cause of urine leakage
- If prolapse of the anterior vaginal wall is diagnosed simultaneously with stress urinary incontinence, then it is imperative to perform plastic surgery of the anterior vaginal wall (vaginoplasty)
- A comprehensive urodynamic study allows you to accurately establish the diagnosis and conduct differential diagnosis with other causes of urinary incontinence
Treatment of stress urinary incontinence
- When slightly severe symptoms appointment of local hormonal drugs as vaginal suppositories and vaginal cream(ovestine)
- The use of biopolymer gels, which are administered endoscopically paraurethral. The operation is performed on an outpatient basis. This technique is recommended for young nulliparous women.
- Sling operations – TOT, TVT, TVT-O, mini slings
Treatment of stress urinary incontinence - TOT sling surgery
The indication for surgery for urinary incontinence is stress urinary incontinence, with or without cystocele and genital prolapse. The main advantage of surgery for urinary incontinence, along with its low trauma, is the ability to control the tension of the loop. As a loop, a prolene tape is used, which has no fixation, that is, free tension is applied. Prolene is not absorbed, encapsulated in tissues without losing its original tensile strength. There are no contraindications to incontinence surgery using a synthetic loop. This indicates the safety of the operation for urinary incontinence using the TOT method.
Urinary incontinence surgery - TOT sling surgery
A urethral catheter is placed in a patient with urinary incontinence. A longitudinal incision is made in the anterior wall of the vagina 3 cm, under the middle urethra. The middle urethra is exposed in layers. Then through a puncture on the right side inner surface the conductor is inserted under the urethra, the end of the loop is attached to it, and the conductor with the loop is brought back. The loop passes through the obturator foramen. Do the same on the left. The tension of the loop is checked, the loop is placed exactly under the urethra, and the wound of the anterior wall of the vagina is sutured. The ends of the loop are cut off, the injection sites are sutured with single sutures. Urinary incontinence surgery completed.




