Medicinal reference book geotar. Factor VII (Coagulation Factor VII) (Factor VII (Coagulation Factor VII))
lyophilisate for preparation. r-ra d / in / in the introduction of 600 IU: fl. 1 PC. in set with solvent, syringe, disposable needle, transfer needle, filtering needle, aeration needle. and transfusion system Reg. No.: P N016158/01
Clinico-pharmacological group:
Blood coagulation factor VII preparation
Release form, composition and packaging
Lyophilisate for solution for intravenous administration white or slightly colored, in the form of powder or friable solid mass.
Excipients: sodium citrate dihydrate, sodium chloride, heparin.
Solvent: water d / i - 10 ml.
Vials (1) complete with a solvent (vial), a disposable syringe, a disposable needle, a transfer needle, a filtering needle, an aeration needle and a transfusion system - packs of cardboard.
Description of the active ingredients of the drug Factor vii (clotting factor vii)»
pharmachologic effect
Factor VII is one of the vitamin K-dependent factors in normal human plasma, a component of the external pathway of the blood coagulation system. It is a factor VIla serine protease zymogen that triggers outer path blood coagulation systems. Concentrate Introduction human factor VII increases the concentration of factor VII in plasma and provides a temporary correction of the defect in the blood coagulation system in patients with factor VII deficiency.
Indications
Treatment and prevention of blood clotting disorders caused by hereditary or acquired factor VII deficiency;
— acute bleeding and prevention of bleeding surgical interventions in patients with congenital factor VII deficiency (hypo- or aproconvertinemia);
- acute bleeding and prevention of bleeding during surgical interventions with acquired factor VII deficiency due to oral anticoagulants;
- deficiency of vitamin K (for example, in violation of its absorption in the gastrointestinal tract, with prolonged parenteral nutrition);
— liver failure(eg, hepatitis, cirrhosis, severe toxic damage liver).
Dosing regimen
Duration replacement therapy and doses depend on the severity of the factor VII deficiency, the location and extent of bleeding or hemorrhage, and clinical condition sick. The prescribed dose of factor VII is calculated in international units (IU) according to current WHO standards for preparations containing factor VII. Plasma factor VII activity can be calculated as a percentage of normal and in international units.
One International Unit of Factor VII activity is equivalent to 1 ml of Factor VII activity in normal human plasma.
The required dose is calculated on the basis of empirical observation, which showed that with the introduction of 1 ME of factor VII per 1 kg of body weight, the activity of factor VII in plasma increases by 1.7%.
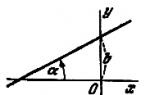
The calculation of the required dose is carried out according to the following formula:
Required dose (ME) = body weight (kg) x desired increase in factor VII activity (%) x 0.6
When determining the dose and frequency of administration of the drug in each case, the clinical effect should be taken into account.
When choosing the interval of administration, it should be taken into account that the half-life of factor VII is very short - approximately 3-5 hours.
If you need to maintain for a long time high level factor VII in plasma, the drug should be administered at intervals of 8-12 hours.
Dose adjustment in liver disease is not required.
Method of administration
A solution for IV administration from Factor VII lyophilisate should be prepared immediately prior to administration. Use only the supplied insertion kit. The solution should be clear or slightly opalescent. Do not use the solution if it is cloudy or contains particulate matter. All used materials and unused solution must be disposed of in accordance with established regulations.
Preparation of a solution from a lyophilized concentrate
1. Heat the closed solvent bottle to room temperature(not higher than 37°С).
2. Remove the protective caps from the Factor VII Concentrate and Diluent vials and disinfect the rubber stoppers on both vials.
3. Turn and then remove the protective packaging from one end of the adapter needle included in the kit. Use the end of the needle to pierce the rubber stopper of the solvent bottle.
4. Carefully remove the protective packaging from the other end of the adapter needle without touching the needle itself.
5. Invert the solvent vial and pierce the rubber stopper of the Factor VII concentrate vial with the free end of the adapter needle. The vacuum will force the solvent into the Factor VII Concentrate vial.
6. Disconnect the vials by removing the adapter needle from the Factor VII concentrate vial. For faster dissolution of the concentrate, the bottle is gently rotated and shaken.
7. For foam deposition after complete dissolution of the concentrate, insert the supplied air needle into the vial. Remove the airway needle after the foam has settled.
In/in jet injection
1. Turn and then remove the protective packaging from the filter needle and put it on a sterile disposable syringe. Draw the solution into a syringe.
2. Disconnect the filter needle from the syringe, put on a butterfly needle or a disposable injection needle and inject the intravenous solution slowly (at a rate of no more than 2 ml / min).
3. When administering at home, the patient should place all used materials in the drug package and hand it over to medical institution where it is observed for control.
IV drip
For intravenous drip, a disposable transfusion system with a filter should be used.
Side effect
Rarely there is a development allergic reactions(such as urticaria, nausea, vomiting, bronchospasm, lowering blood pressure), in some cases - severe anaphylaxis (including shock).
AT rare cases fever was noted. When treated with prothrombin complex factors, one of which is factor VII, thromboembolic complications are possible, especially in cases where high doses of the drug are prescribed and / or in patients with risk factors for thromboembolism.
Contraindications
- syndrome of disseminated intravascular coagulation (DIC) and / or hyperfibrinolysis until the underlying causes are eliminated;
- a history of heparin-induced thrombocytopenia;
- age up to 6 years;
— hypersensitivity to the drug or to any of its components.
Due to the risk of developing thromboembolic complications, the drug with special care should be used in patients with a history of coronary artery disease, myocardial infarction, liver disease, and in patients with postoperative period, newborns and persons with high risk development of thromboembolism or DIC. In these cases, it is necessary to correlate possible benefit from the use of Factor VII with the risk of developing these complications.
Pregnancy and lactation
The safety of Factor VII during pregnancy has not been confirmed by controlled clinical trials. Therefore, Factor VII can be administered during pregnancy and lactation only under strict indications.
Application for violations of liver function
With caution, the drug should be prescribed for liver diseases.
Application for children
Contraindicated in children under 6 years of age.
special instructions
Since Factor VII is a protein drug, allergic reactions may occur. Patients should be informed about early symptoms allergies such as urticaria (including generalized), chest tightness, wheezing, drop in blood pressure and anaphylaxis. If these symptoms appear, patients should immediately stop treatment and contact their doctor.
With the development of shock, one should act in accordance with the established this moment shock treatment guidelines.
Based on the experience with the human plasma prothrombin complex, we can talk about an increased risk of thromboembolic complications and DIC in patients receiving human plasma factor VII.
Theoretically, factor VII replacement therapy could lead to the development of factor VII inhibitors in the patient. However, up to now in clinical practice no such case has been described.
The amount of sodium in the maximum daily dose may exceed 200 mg, which should be considered when used in patients on a low sodium diet.
Factor VII is made from human plasma. With the introduction of drugs made from human blood or plasma, the possibility of virus transmission cannot be completely excluded. This also applies to pathogens whose nature is currently unknown.
The risk of virus transmission is minimized as a result of the implementation of a number of security measures, namely:
— selection of donors based on data medical examination and screening of blood and plasma of each donor, as well as plasma pools for HBsAg and antibodies to HIV and hepatitis C viruses;
- testing of plasma pools for the presence of genomic material of hepatitis A, B and C, HIV-1 and HIV-2 viruses, as well as parvovirus B19;
— application of virus inactivation/removal methods in the manufacturing process. The effectiveness of these methods against hepatitis A, B and C, HIV-1 and HIV-2 viruses has been established on pathogen viruses and/or model viruses.
However, the effectiveness of the applied methods of inactivation/removal of viruses may be insufficient against some non-enveloped viruses, for example, parvovirus B19, as well as against currently unknown viruses. Infection with parvovirus B19 can be dangerous for pregnant women (infection of the fetus), as well as for people with immunodeficiency or increased production of red blood cells (for example, with hemolytic anemia).
Hepatitis A and B vaccination is recommended for patients receiving human plasma factor VII.
There are currently insufficient data to recommend the use of Factor VII in children under 6 years of age.
Influence on the ability to drive vehicles and control mechanisms
There was no effect on the ability to drive a car and moving mechanisms.
Overdose
When using large doses of drugs containing factor VII, there were cases of myocardial infarction, disseminated intravascular coagulation syndrome, venous thrombosis and thromboembolism pulmonary artery. Therefore, in the event of an overdose in patients with risk factors for thromboembolic complications or disseminated intravascular coagulation, the likelihood of developing these complications increases.
drug interaction
Terms of dispensing from pharmacies
The drug is dispensed by prescription.
Terms and conditions of storage
The drug should be stored out of the reach of children at a temperature of 2 ° to 8 ° C. Shelf life - 3 years.
drug interaction
INTERACTIONS WITH OTHER DRUGS
No interactions of human plasma Factor VII with other drugs have been noted.
Prior to administration, Factor VII should not be mixed with other drugs. Using venous catheter it is recommended to wash it with isotonic saline before and after the administration of Factor VII.
Impact on laboratory parameters:
In patients receiving large doses Factor VII, when conducting coagulological tests that are sensitive to heparin, the presence of heparin in the preparation should be taken into account. If necessary, the effect of heparin can be neutralized by adding protamine to the test sample.
Carried out mainly by proteins called plasma factors blood clotting. Plasma coagulation factors are procoagulants whose activation and interaction lead to the formation of a fibrin clot.
According to the International Nomenclature, plasma coagulation factors are indicated by Roman numerals, with the exception of von Willebrand, Fletcher and Fitzgerald factors. To indicate the activated factor, the letter "a" is added to these numbers. In addition to the numerical designation, other names of clotting factors are also used - according to their function (for example, factor VIII- antihemophilic globulin), by the names of patients with a newly discovered deficiency of one or another factor (factor XII - Hageman factor, factor X - Stuart-Prauer factor), less often - by the names of the authors (for example, von Willebrand factor).
Below are the main blood coagulation factors and their synonyms according to the international nomenclature and their main properties in accordance with the literature and special studies.
Fibrinogen (factor I)
Fibrinogen is synthesized in the liver and cells of the reticuloendothelial system (in bone marrow, spleen, lymph nodes etc.). In the lungs, under the action of a special enzyme - fibrinogenase or fibrinodestructase - fibrinogen is destroyed. The content of fibrinogen in plasma is 2 - 4 g / l, the half-life is 72 - 120 hours. The minimum level required for hemostasis is 0.8 g/L.
Under the influence of thrombin, fibrinogen is converted into fibrin, which forms a mesh basis of a thrombus that clogs a damaged vessel.
Prothrombin (factor II)
Prothrombin is synthesized in the liver with the participation of vitamin K. The content of prothrombin in plasma is about 0.1 g / l, the half-life is 48 - 96 hours.
The level of prothrombin, or its functional usefulness, decreases with endogenous or exogenous vitamin K deficiency, when defective prothrombin is formed. The rate of blood clotting is disturbed only when the concentration of prothrombin is below 40% of the norm.
AT vivo during blood coagulation under the action of and, as well as with the participation of factors V and Xa (activated factor X), united by the general term "prothrombinase", prothrombin turns into thrombin. The process of converting prothrombin to thrombin is rather complicated, since during the reaction a number of derivatives of prothrombin, autoprothrombins and, finally, various types thrombin (thrombin C, thrombin E), which have procoagulant, anticoagulant and fibrinolytic activity. The resulting thrombin C - the main product of the reaction - contributes to the coagulation of fibrinogen.
Tissue thromboplastin (factor III)
Tissue thromboplastin is a thermostable lipoprotein found in various organs - in the lungs, brain, kidneys, heart, liver, skeletal muscles. The tissues do not contain active state, and in the form of a precursor - prothromboplastin. Tissue thromboplastin, when interacting with plasma factors (VII, IV), is able to activate factor X, participates in the external pathway for the formation of prothrombinase, a complex of factors that convert to thrombin.
Calcium ions (factor IV)
Calcium ions are involved in all three phases of blood coagulation: in the activation of prothrombinase (phase I), the conversion of prothrombin into thrombin (phase II) and fibrinogen into fibrin (phase III). Calcium is able to bind heparin, thereby accelerating blood clotting. In the absence of calcium, platelet aggregation and retraction are impaired blood clot. Calcium ions inhibit fibrinolysis.
Proaccelerin (factor V)
Proaccelerin (factor V, plasma AC-globulin or labile factor) is formed in the liver, but, unlike other hepatic factors of the prothrombin complex (II, VII, and X), does not depend on vitamin K. It is easily destroyed. The content of factor V in plasma - 12 - 17 units / ml (about 0.01 g / l), half-life - 15 - 18 hours. The minimum level required for hemostasis is 10-15%.
Proaccelerin is necessary for the formation of internal (blood) prothrombinase (activates factor X) and for the conversion of prothrombin to thrombin.
Accelerin (factor VI)
Accelerin (factor VI or serum AC-globulin) is the active form of factor V. Excluded from the nomenclature of coagulation factors, only the inactive form of the enzyme is recognized - factor V (proaccelerin), which, when traces of thrombin appear, turns into active form.
Proconvertin, convertin (factor VII)
Proconvertin is synthesized in the liver with the participation of vitamin K. It remains in stabilized blood for a long time, and is activated by a wetted surface. The content of factor VII in plasma is about 0.005 g / l, the half-life is 4 - 6 hours. The minimum level required for hemostasis is 5-10%.
Convertin, the active form of the factor, plays a major role in the formation of tissue prothrombinase and in the conversion of prothrombin to thrombin. Factor VII activation occurs at the very beginning chain reaction upon contact with a foreign surface. During the clotting process, proconvertin is not consumed and is stored in the serum.
Antihemophilic globulin A (factor VIII)
Antihemophilic globulin A is produced in the liver, spleen, endothelial cells, leukocytes, and kidneys. The content of factor VIII in plasma is 0.01 - 0.02 g / l, the half-life is 7 - 8 hours. The minimum level required for hemostasis is 30-35%.
Antihemophilic globulin A is involved in the "internal" pathway for the formation of prothrombinase, enhancing the activating effect of factor IXa (activated factor IX) on factor X. Factor VIII circulates in the blood, being associated with.
Antihemophilic globulin B (Christmas factor, factor IX)
Antihemophilic globulin B (Christmas factor, factor IX) is formed in the liver with the participation of vitamin K, is thermostable, and remains in plasma and serum for a long time. The content of factor IX in plasma is about 0.003 g/L. The half-life is 7-8 hours. The minimum level required for hemostasis is 20-30%.
Antihemophilic globulin B is involved in the "internal" pathway of prothrombinase formation, activating factor X in combination with factor VIII, calcium ions and platelet factor 3.
Stuart-Prower Factor (Factor X)
Stuart-Prower factor is produced in the liver in an inactive state, activated by trypsin and an enzyme from viper venom. K-vitamin-dependent, relatively stable, half-life - 30 - 70 hours. The content of factor X in plasma is about 0.01 g / l. The minimum level required for hemostasis is 10-20%.
The Stuart-Prower factor (factor X) is involved in the formation of prothrombinase. AT modern scheme In blood clotting, active factor X (Xa) is the central factor in prothrombinase, which converts prothrombin to thrombin. Factor X is converted into the active form under the influence of factors VII and III (external, tissue, prothrombinase formation pathway) or factor IXa together with VIIIa and phospholipid with the participation of calcium ions (internal, blood, prothrombinase formation pathway).
Plasma thromboplastin precursor (factor XI)
The plasma thromboplastin precursor (factor XI, Rosenthal factor, antihemophilic factor C) is synthesized in the liver and is thermolabile. The content of factor XI in plasma is about 0.005 g / l, the half-life is 30 - 70 hours.
The active form of this factor (XIa) is formed with the participation of factors XIIa, and. Form XIa activates factor IX, which is converted to factor IXa.
Hageman Factor (Factor XII, Contact Factor)
Hageman factor (factor XII, contact factor) is synthesized in the liver, produced in an inactive state, the half-life is 50-70 hours. The content of the factor in plasma is about 0.03 g/l. Bleeding does not occur even with very deep factor deficiency (less than 1%).
It is activated upon contact with the surface of quartz, glass, cellite, asbestos, barium carbonate, and in the body - upon contact with the skin, collagen fibers, chondroitin sulfuric acid, saturated micelles fatty acids. Factor XII activators are also Fletcher's factor, kallikrein, factor XIa, plasmin.
The Hageman factor is involved in the "internal" pathway of prothrombinase formation by activating factor XI.
Fibrin stabilizing factor (factor XIII, fibrinase, plasma transglutaminase)
Fibrin-stabilizing factor (factor XIII, fibrinase, plasma transglutaminase) is determined in vascular wall, platelets, erythrocytes, kidneys, lungs, muscles, placenta. In plasma, it is in the form of a proenzyme combined with fibrinogen. The active form is converted under the influence of thrombin. It is contained in plasma in an amount of 0.01 - 0.02 g / l, the half-life is 72 hours. The minimum level required for hemostasis is 2-5%.
Fibrin-stabilizing factor is involved in the formation of a dense clot. It also influences the adhesion and aggregation of platelets.
Willebrand factor (antihemorrhagic vascular factor)
Willebrand factor (antihemorrhagic vascular factor) is synthesized by vascular endothelium and megakaryocytes, and is found in plasma and platelets.
The von Willebrand factor serves as an intravascular carrier protein for factor VIII. The binding of von Willebrand factor to factor VIII stabilizes the latter molecule, increases its half-life inside the vessel, and promotes its transport to the site of injury. Other physiological role The relationship between factor VIII and von Willebrand factor lies in the ability of von Willebrand factor to increase the concentration of factor VIII at the site of vessel damage. Since circulating von Willebrand factor binds to both exposed subendothelial tissues and stimulated platelets, it directs factor VIII to the affected area, where the latter is required for factor X activation with the participation of factor IXa.
Fletcher factor (plasma prekallikrein)
Fletcher factor (plasma prekallikrein) is synthesized in the liver. The content of the factor in plasma is about 0.05 g/L. Bleeding does not occur even with very deep factor deficiency (less than 1%).
Participates in the activation of factors XII and IX, plasminogen, converts kininogen to kinin.
Fitzgerald factor (plasma kininogen, Flojek factor, Williams factor)
Fitzgerald factor (plasma kininogen, Flojek factor, Williams factor) is synthesized in the liver. The content of the factor in plasma is about 0.06 g/L. Bleeding does not occur even with very deep factor deficiency (less than 1%).
Participates in the activation of factor XII and plasminogen.
Literature:
- Handbook of Clinical Laboratory Research Methods. Ed. E. A. Kost. Moscow, "Medicine", 1975
- Barkagan Z. S. Hemorrhagic diseases and syndromes. - Moscow: Medicine, 1988
- Gritsyuk A. I., Amosova E. N., Gritsyuk I. A. Practical hemostasiology. - Kyiv: Health, 1994
- Shiffman F. J. Blood Pathophysiology. Translation from English - Moscow - St. Petersburg: "Publishing house BINOM" - "Nevsky Dialect", 2000
- Directory " Laboratory methods research in the clinic" under the editorship of Prof. V. V. Menshikov. Moscow, "Medicine", 1987
- Study of the blood system in clinical practice. Ed. G. I. Kozints and V. A. Makarov. - Moscow: Triada-X, 1997
Filterable List
Active substance:
Instructions for medical use
Factor VII (Blood Clotting Factor VII)
Instructions for medical use- RU No. P N016158/01
Last Modified Date: 10.05.2016
Dosage form
Lyophilizate for solution for intravenous administration
Compound
Composition (for 1 bottle):
Active ingredient:
Factor VII 600 ME
As plasma protein 50-200 mg/vial
Auxiliary ingredients:
Sodium citrate dihydrate 40 mg
Sodium chloride 80 mg
Heparin sodium 250 ME
Solvent:
Water for injections 10 ml
Description of the dosage form
Lyophilisate: white or slightly colored powder or friable solid mass.
Solvent: clear, colorless liquid.
Reconstituted solution: clear to slightly opalescent, colorless to yellowish color solution.
Pharmacological group
Hemostatic agent
Pharmacodynamics
Factor VII is one of the vitamin K-dependent factors in normal human plasma, a component of the extrinsic pathway of the blood coagulation system. It is a single chain glycoprotein with molecular weight about 50,000 daltons. Factor VII is a zymogen for the factor Vila serine protease (active serine protease) that triggers the extrinsic pathway of the blood coagulation system. The tissue factor-factor VIIa complex activates coagulation factors IX and X, resulting in the formation of factors IXa and Xa. With further deployment of the coagulation cascade, thrombin is formed, fibrinogen is converted to fibrin, and a clot is formed. Normal thrombin formation is also extremely important for platelet function as part of the hemostasis system. Hereditary factor VII deficiency is an autosomal recessive disorder. The use of human factor VII provides an increase in plasma concentration of factor VII and can temporarily eliminate the defect in blood coagulation in patients with factor VII deficiency.
Pharmacokinetics
With intravenous administration of factor VII, its concentration in the patient's blood plasma rises to 60-100%.
The half-life is about 3-5 hours.
Indications
The drug Factor VII is indicated:
- in the treatment of blood clotting disorders caused by isolated hereditary factor VII deficiency;
- for the prevention of blood clotting disorders caused by isolated hereditary factor VII deficiency, with a history of bleeding and a residual concentration of factor VII below 25% (0.25 IU / ml).
The drug does not contain significant amounts of factor VIIa and should not be used in patients with hemophilia with inhibitors.
Contraindications
- hypersensitivity to active substance or any component of the drug;
- high risk of thrombosis or disseminated intravascular coagulation (DIC);
- a known allergy to heparin or a history of heparin-induced thrombocytopenia;
- children under 6 years of age (currently available data are insufficient to recommend the use medicinal product Factor VII in children under 6 years of age).
Use during pregnancy and lactation
The effect of Factor VII on fertility has not been studied in controlled clinical trials.
Human factor safety coagulation VII when used during pregnancy has not been confirmed by controlled clinical studies.
Data obtained in animal experiments do not allow to evaluate the safety of the drug for pregnant women, the effect on the development of the embryo and fetus, childbirth or postnatal development. The physician must carefully evaluate the expected benefit and possible risk and prescribe Factor VII during pregnancy and during breastfeeding only under strict guidelines.
See section " special instructions”, which contains information about the risks associated with potential danger infection of pregnant women with parvovirus B19.
Dosage and administration
Treatment with Factor VII should only be carried out by a physician experienced in the use of clotting factor replacement therapy.
Factor VII is administered intravenously as intermittent injections or infusions.
Reconstitution of the Factor VII preparation should be carried out immediately before use. When used as an infusion, only the supplied infusion set should be used.
Recovery of lyophilisate
1. Warm unopened vial of solvent to room temperature, but no more than 37°C.
2. Remove the protective discs from the lyophilisate and solvent vials (Fig. A) and wipe the stoppers of both vials.
3. Remove, by rotating and removing, the protective cover from one end of the supplied transfer needle (Fig. B). Insert an open needle through the rubber stopper into the diluent vial (Figure B).
4. Remove the protective coating from the other end of the transfer needle without touching the surface of the needle.
5. Invert the solvent vial vertically over the concentrate vial and insert the free end of the transfer needle through the rubber stopper of the concentrate vial (Fig. D). The solvent will enter the concentrate vial under vacuum.
6. Separate the two vials by removing the needle from the stopper of the concentrate vial (Fig. D). Gently shake and swirl the concentrate vial to promote dissolution.
7. After reconstitution is complete, insert the supplied aeration needle (Fig. E) and allow the foam to settle completely. Remove the aeration needle.
8. Prior to administration, the resulting concentrate should be carefully examined for the presence of foreign particles and discoloration (the concentrate may be colorless or have a yellowish color).
In case of detection of foreign particles, discoloration or turbidity, the drug should not be administered!
The drug must be used immediately after recovery.
Method of administration
1. Remove, by rotating and removing, the protective cover from one end of the supplied filter needle, and place it on a sterile disposable syringe. Draw the solution into the syringe (Fig. G).
2. Disconnect the filter needle from the syringe and perform a slow intravenous administration solution using a transfusion system (or the included disposable needle).
Do not exceed the infusion rate of 2 ml/min!
Doses and duration of replacement therapy depend on the severity of factor VII deficiency, the location and severity of bleeding episodes, and the clinical condition of the patient. The association between factor VII residual levels and bleeding tendency is less clear in some patients than in classical hemophilia.
The number of Factor VII units administered is expressed in International Units (IU) according to the current WHO standard for Factor VII preparations. Plasma Factor VII activity is expressed either as a percentage (relative to normal plasma) or in International Units (relative to International Standard factor VII plasma).
One International Unit (IU) of factor VII activity is equivalent to the amount of factor VII activity in 1 ml of normal human plasma.
Based on the empirical observation that 1 International Unit (IU) of factor VII per kilogram of body weight increases plasma factor VII activity by approximately 1.9% (0.019 IU/mL) relative to normal level activity.
The required dose is determined using the following formula:
Required dose (ME) = body weight (kg) × desired increase in factor VII activity (IU/mL) × 53* (unit divided by observed recovery (mL/kg))
*(because 1: 0.019 = 52.6)
In each individual case, the amount of the drug to be administered and the frequency of application should always be correlated with clinical efficacy. This is particularly important in the treatment of factor VII deficiency, since an individual's tendency to bleed does not depend strictly on plasma factor VII activity as measured by laboratory tests. Individual dosage recommendations for Factor VII should be based on regular measurements of factor VII plasma concentrations and ongoing monitoring of the patient's clinical status. The intervals between doses should take into account the short half-life of factor VII from the circulatory bed, which is from 3 to 5 hours.
When using the drug Factor VII in the form of intermittent injections / infusions, it is advisable to do the intervals between doses from 6 to 8 hours. In general, the treatment of factor VII deficiency requires (depending on activity in normal plasma) lower doses of the deficient factor compared to classical hemophilia (hemophilia A and B). The table below shows exemplary recommendations on the use of intermittent injections/infusions based on the limited clinical experience available.
| Degree of bleeding / Type of surgery | Required factor VII concentration IU/mL* | Frequency of administration (hours) / Duration of therapy (days) |
| light bleeding | 0,10-0,20 | single dose |
| heavy bleeding | (lowest-highest concentration) | Within 8-10 days or up to complete cessation bleeding** |
| 0,20-0,30 | single dose before surgical operation or, if the perceived risk of bleeding is more obvious, until the wound heals* | |
| Major surgical interventions | Before surgery > 0.50, then 0.25-0.45 (lowest-highest concentrations) | Within 8-10 days or until the wound is completely healed** |
* 1 IU/mL=100 IU/dL=100% normal plasma. Plasma factor VII activity is expressed either as a percentage (relative to the content in normal plasma, taken as 100%), or in International Units (relative to international standard for factor VII in plasma).
** Based clinical assessment in each case, provided that adequate hemostasis is achieved towards the end of treatment, lower doses may be sufficient. The intervals between doses should be selected taking into account short period the elimination half-life of factor VII from the circulatory bed, which is approximately 3 to 5 hours. Support if necessary high concentrations factor VII over a long period of time doses should be administered at intervals of 8-12 hours.
Unused drug and waste material must be disposed of in accordance with local requirements.
Side effects
Adverse Effects Observed in Clinical Studies
Adverse reactions encountered during the course of clinical research, are listed according to the following gradation: according to the following gradation: very often (> 1/10); often (> 1/100<1/10); нечасто (>1/1000<1/100); редко (> 1/10 000<1/1000); очень редко (<1/10 000, включая единичные сообщения).
The table below summarizes the adverse reactions reported in a clinical study of 57 adult and pediatric patients with hereditary factor VII deficiency who were treated with Factor VII for acute bleeding control, during surgery, and for long-term bleeding prevention. In this study, Factor VII was administered for 8234 days.
| Organ system | Preferred MedDRA Term | Frequency per patient a | Frequency in % | Frequency on the day of administration b | Frequency in % |
| Vascular disorders | Hyperemia | Often | 1/57 (1,75 %) | Rarely | 1/8234 (0,01 %) |
| Skin and subcutaneous tissue disorders | Rash | Often | 1/57 (1,75 %) | Rarely | 1/8234 (0,01 %) |
| General disorders and reactions at the injection site | Hyperthermia | Often | 1/57 (1,75 %) | Rarely | 1/8234 (0,01 %) |
| Chest pain | Often | 1/57 (1,75 %) | Rarely | 2/8234 (0,01 %) | |
| Disturbance of well-being c | Often | 1/57 (1,75 %) | Rarely | 1/8234 (0,01 %) |
a - Rate per Patient was determined based on the number of patients who experienced this adverse event, assessed by the investigator as at least possibly related to the administration of the drug, and assessed in the same way by Baxter Healthcare Corporation.
b = "Frequency per day of administration" was determined based on the total number of observations of this adverse event, assessed by the investigator as at least possibly related to the administration of the drug, and thus estimated by Baxter Healthcare Corporation.
c - "Violation of well-being" - the applied term, implying a fuzzy perception.
Undesirable effects observed during post-registration use
The following adverse effects have been reported in post-marketing experience, listed according to the MedDRA Organ System Classification in ascending order of severity, where applicable.
Blood and lymphatic system disorders: factor VII* inhibition.
*-Coded under the preferred MedDRA term for the presence of anti-factor VII antibodies.
Immune system disorders: hypersensitivity reactions.
Mental disorders: confusion, insomnia, restlessness.
Nervous system disorders: cerebral vein thrombosis, dizziness, sensory disturbance, headache.
Cardiovascular disorders: arrhythmia, hypotension, deep vein thrombosis, superficial vein thrombosis, facial flushing.
Respiratory, thoracic and mediastinal disorders: bronchospasm, shortness of breath.
Gastrointestinal disorders: diarrhea, nausea.
Skin and subcutaneous tissue disorders: itching.
General disorders and reactions at the injection site: chest discomfort.
Class-Specific Reactions
When using factor VII preparations and prothrombin complex preparations containing factor VII, the following adverse events were noted: stroke, myocardial infarction, arterial thrombosis, pulmonary embolism, disseminated intravascular coagulation, allergic or anaphylactic reactions, urticaria, vomiting, fever.
Precautionary measures
When conducting coagulation tests sensitive to heparin in patients receiving high doses of Factor VII, the presence of heparin in the preparation should be taken into account.
special instructions
When using preparations containing factor VII, the development of hypersensitivity reactions, including anaphylactic reactions, was noted. Patients and their loved ones should be informed about the early signs of hypersensitivity reactions. If such symptoms occur, patients should be advised to immediately discontinue the use of the drug and contact their doctor.
If allergic and / or anaphylactic reactions occur, the administration should be stopped immediately. In case of shock, standard medical measures should be taken.
Standard measures for the prevention of infections resulting from the use of medicinal products derived from human blood or plasma include the selection of donors, the screening of material donated by individual donors and plasma pools for specific markers of infection, and the introduction of effective virus inactivation/removal steps into production . Despite this, when using medicinal products prepared from human blood or plasma, the risk of transmission of infectious diseases, including those caused by unknown viruses or other pathogens, cannot be completely excluded.
Applied technologies for the removal and inactivation of pathogens may be of limited effectiveness against some non-enveloped viruses, in particular, parvovirus B19. Infection with parvovirus B19 can be dangerous for pregnant women (infection of the fetus) and patients with immunodeficiency or increased breakdown of red blood cells (in particular, with hemolytic anemia).
Appropriate vaccination (against hepatitis A and B) may be recommended for patients who are regularly treated with plasma-derived Factor VII.
Each time Factor VII is administered, it is strongly recommended that the name and batch number of the drug be recorded so that the relationship between the administration of the drug and the patient's condition can be traced.
During therapy with drugs containing factor VII, there is a risk of developing thromboembolic complications and DIC. Thrombosis, including deep vein thrombosis, and thrombophlebitis have been observed during treatment with Factor VII. Patients receiving Factor VII therapy should be closely monitored due to the possibility of developing signs and symptoms of thromboembolic complications and DIC.
Due to the risk of thromboembolic complications and DIC, particularly rigorous monitoring should be performed when administering human factor VII to patients with coronary heart disease, liver disease, prior to surgery, neonatal neonates, or other patients.
Replacement therapy with human factor VII can lead to the formation of circulating antibodies that inhibit factor VII. If such inhibitors appear, this condition manifests itself as an insufficient clinical response.
Influence on the ability to drive vehicles and other mechanisms
There is no information on the effect of Factor VII on the ability to drive a car and use complex machinery that requires increased attention.
Release form
Lyophilisate for solution for intravenous administration 600 ME
600 IU of the drug in a glass vial (type II, EP) and 10 ml of solvent in a glass vial (type I, EP) in a carton box together with a set for dissolution and administration (disposable syringe, disposable needle, transfer needle, filter needle , aeration needle, transfusion system) and instructions for use
Storage conditions
At temperatures from 2 to 8°C.
Keep out of the reach of children.
Best before date
Do not use after the expiry date stated on the packaging.
Terms of dispensing from pharmacies
By prescription.
Factor VII (Blood coagulation factor VII) - instructions for medical use - RU No. P N016158 / 01 dated 2009-12-15
Synonyms of nosological groups
| Category ICD-10 | Synonyms of diseases according to ICD-10 |
|---|---|
| D68.2 Hereditary deficiency of other coagulation factors | Coagulation factor II deficiency |
| Coagulation factor VII deficiency | |
| Coagulation factor X deficiency | |
| Coagulation factor XII deficiency | |
| Stuart-Prower factor deficiency | |
| Dysfibrinogenemia | |
| Hereditary anomalies of the Stuart-Prower factor (factor X) | |
| Hereditary anomalies of the Hageman factor (factor XII) | |
| Hereditary deficiency of AT-III | |
| Plasma coagulation factor deficiency | |
| E56.1 Vitamin K deficiency | Vitamin K deficiency |
| Vitamin K1 deficiency | |
| K72.9 Liver failure, unspecified | Latent hepatic encephalopathy |
| Acute liver failure | |
| Acute hepatic-renal failure | |
| Liver failure | |
| Hepatic precoma | |
| Z100* CLASS XXII Surgical practice | Abdominal surgery |
| Adenomectomy | |
| Amputation | |
| Angioplasty of coronary arteries | |
| Angioplasty of the carotid arteries | |
| Antiseptic skin treatment for wounds | |
| Antiseptic hand treatment | |
| Appendectomy | |
| Atherectomy | |
| Balloon coronary angioplasty | |
| Vaginal hysterectomy | |
| Crown bypass | |
| Interventions on the vagina and cervix | |
| Bladder interventions | |
| Intervention in the oral cavity | |
| Restorative and reconstructive operations | |
| Hand hygiene of medical personnel | |
| Gynecological surgery | |
| Gynecological interventions | |
| Gynecological operations | |
| Hypovolemic shock during surgery | |
| Disinfection of purulent wounds | |
| Disinfection of wound edges | |
| Diagnostic interventions | |
| Diagnostic procedures | |
| Diathermocoagulation of the cervix | |
| Long-term surgery | |
| Replacement of fistula catheters | |
| Infection during orthopedic surgery | |
| Artificial heart valve | |
| cystectomy | |
| Brief outpatient surgery | |
| Short-term operations | |
| Short term surgical procedures | |
| Cricothyrotomy | |
| Blood loss during surgery | |
| Bleeding during surgery and in the postoperative period | |
| Culdocentesis | |
| Laser coagulation | |
| Laser coagulation | |
| Laser coagulation of the retina | |
| Laparoscopy | |
| Laparoscopy in gynecology | |
| CSF fistula | |
| Minor gynecological surgeries | |
| Minor surgical interventions | |
| Mastectomy and subsequent plasty | |
| Mediastinotomy | |
| Microsurgical operations on the ear | |
| Mucogingival operations | |
| Suturing | |
| Minor surgical interventions | |
| Neurosurgical operation | |
| Immobilization of the eyeball in ophthalmic surgery | |
| Orchiectomy | |
| Complications after tooth extraction | |
| Pancreatectomy | |
| Pericardectomy | |
| The period of rehabilitation after surgical operations | |
| The period of convalescence after surgical interventions | |
| Percutaneous transluminal coronary angioplasty | |
| Pleural thoracocentesis | |
| Pneumonia postoperative and post-traumatic | |
| Preparation for surgical procedures | |
| Preparing for surgery | |
| Preparation of the surgeon's hands before surgery | |
| Preparing the colon for surgery | |
| Postoperative aspiration pneumonia in neurosurgical and thoracic operations | |
| Postoperative nausea | |
| Postoperative bleeding | |
| Postoperative granuloma | |
| Postoperative shock | |
| Early postoperative period | |
| Myocardial revascularization | |
| Resection of the apex of the tooth root | |
| Resection of the stomach | |
| Bowel resection | |
| Uterine resection | |
| Liver resection | |
| Resection of the small intestine | |
| Resection of a part of the stomach | |
| Reocclusion of the operated vessel | |
| Bonding tissue during surgery | |
| Removal of stitches | |
| Condition after eye surgery | |
| Condition after surgery | |
| Condition after surgical interventions in the nasal cavity | |
| Condition after resection of the stomach | |
| Condition after resection of the small intestine | |
| Condition after tonsillectomy | |
| Condition after removal of the duodenum | |
| Condition after phlebectomy | |
| Vascular surgery | |
| Splenectomy | |
| Sterilization of the surgical instrument | |
| Sterilization of surgical instruments | |
| Sternotomy | |
| Dental operations | |
| Dental intervention on periodontal tissues | |
| Strumectomy | |
| Tonsillectomy | |
| Thoracic Surgery | |
| Thoracic surgery | |
| Total gastrectomy | |
| Transdermal intravascular coronary angioplasty | |
| Transurethral resection | |
| Turbinectomy | |
| Removal of a tooth | |
| Cataract removal | |
| Removal of cysts | |
| Tonsil removal | |
| Removal of fibroids | |
| Removal of mobile milk teeth | |
| Removal of polyps | |
| Removal of a broken tooth | |
| Removal of the body of the uterus | |
| Suture removal | |
| Urethrotomy | |
| CSF fistula | |
| Frontoethmoidogaimorotomy | |
| Surgical infection | |
| Surgical treatment of chronic leg ulcers | |
| Surgery | |
| Surgery in the anus | |
| Surgical operation on the large intestine | |
| Surgical practice | |
| surgical procedure | |
| Surgical interventions | |
| Surgical interventions on the gastrointestinal tract | |
| Surgical interventions on the urinary tract | |
| Surgical interventions on the urinary system | |
| Surgical interventions on the genitourinary system | |
| Surgical interventions on the heart | |
| Surgical manipulations | |
| Surgical operations | |
| Surgical operations on the veins | |
| Surgical intervention | |
| Surgical intervention on the vessels | |
| Surgical treatment of thrombosis | |
| Surgery | |
| Cholecystectomy | |
| Partial resection of the stomach | |
| Transperitoneal hysterectomy | |
| Percutaneous transluminal coronary angioplasty | |
| Percutaneous transluminal angioplasty | |
| Bypass coronary arteries | |
| Tooth extirpation | |
| Extraction of milk teeth | |
| Pulp extirpation | |
| extracorporeal circulation | |
| Tooth extraction | |
| Extraction of teeth | |
| Cataract Extraction | |
| Electrocoagulation | |
| Endourological interventions | |
| Episiotomy | |
| Ethmoidectomy |
|
Active form function |
||
|
fibrinogen |
Forms fibrin gel |
|
|
Prothrombin |
Activates fibrinogen (serine protease) |
|
|
tissue thromboplastin |
Stimulates the activation of f VII (extrinsic pathway; substrate protein) |
|
|
Calcium ions |
Necessary for the interaction of coagulation factors with the phospholipid surface |
|
|
Proalekrin |
Stimulates the activation of f II (substrate protein) |
|
|
Proconvertin |
Activates fX (serine protease) |
|
|
Antihemophilic factor A |
Stimulates the activation of fX (substrate protein) |
|
|
Antihemophilic factor B |
Stimulates fX (serine protease) |
|
|
Stuart-Prower factor |
Activates f II (serine protease) |
|
|
Plasma thromboplastin precursor |
Activates f IX (serine protease) |
|
|
Hageman factor |
Activates f XI (serine protease) |
|
|
fibrin stabilizing factor |
Stabilizes the fibrin network (transglutaminase) |
|
|
Prekallikrein (Fletcher factor) |
Plasminogen activation |
|
|
High molecular weight kininogen (Fitzgerald-Floget factor) |
contact activation factor |
|
|
Protein C |
Inactivation of activated factors V and XIII |
|
|
Protein S |
Stimulates factor inactivation by activated protein C |
|
|
Willebrand factor |
Mediates platelet binding to subendothelium |
Most plasma coagulation factors are produced in the liver. For the synthesis of some of them (II, VII, IX, X), vitamin K is needed, which is contained in plant foods and synthesized by the intestinal microflora. With a lack or decrease in the activity of blood coagulation factors, pathological bleeding can be observed. This can occur with severe and degenerative liver diseases, with vitamin K deficiency. Vitamin K is a fat-soluble vitamin, so its deficiency can be detected when fat absorption in the intestine is inhibited, for example, when bile formation is reduced. Endogenous deficiency of vitamin K is also observed when the intestinal microflora is suppressed by antibiotics. A number of diseases in which there is a deficiency of plasma factors is hereditary. An example is the various forms of hemophilia, which only affect men but are transmitted by women.
The substances found in platelets are called platelet, or lamellar, blood coagulation factors. They are denoted by Arabic numerals. The most important platelet factors include: PF-3 (platelet thromboplastin) - a lipid-protein complex, on which, as on a matrix, hemocoagulation occurs, PF-4 - an antiheparin factor, PF-5 - due to which platelets are capable of adhesion and aggregation, PF- 6 (thrombostenin) is an actinomyosin complex that provides thrombus retraction, PF-10 is serotonin, PF-11 is an aggregation factor representing a complex of ATP and thromboxane.
Similar substances have been discovered in both erythrocytes and leukocytes. During transfusion of incompatible blood, Rhesus conflict between mother and fetus, there is a massive destruction of red blood cells and the release of these factors into the plasma, which is the cause of intense intravascular coagulation. In many inflammatory and infectious diseases, disseminated (common) intravascular coagulation (DIC) also occurs. caused by leukocyte coagulation factors.
According to modern concepts, 2 mechanisms are involved in stopping bleeding: vascular-platelet and coagulation.
Vascular-platelet hemostasis
Thanks to this mechanism, bleeding from small vessels with low blood pressure is stopped. In case of injury, a reflex spasm of damaged blood vessels is observed, which is further supported by vasoconstrictor substances (serotonin, norepinephrine, adrenaline) released from platelets and damaged tissue cells. The inner wall of the vessels at the site of damage changes its charge from negative to positive. Due to the ability to adhere under the influence of the von Willebrand factor contained in the subendothelium and platelets, negatively charged platelets adhere to a positively charged wound surface. Almost simultaneously, aggregation occurs - crowding and gluing of platelets with the formation of a platelet plug, or thrombus. First, under the influence of ATP, ADP and adrenaline of platelets and erythrocytes, a loose platelet plug is formed through which plasma passes (reversible aggregation). Then platelets lose their structure and merge into a uniform mass, forming a plug impermeable to plasma (irreversible aggregation). This reaction proceeds under the action of thrombin, which is formed in small amounts under the action of tissue thromboplastin. Thrombin destroys the platelet membrane, which leads to the release of serotonin, histamine, enzymes, and blood coagulation factors from them. Plate factor 3 gives rise to the formation of platelet prothrombinase, which leads to the formation of a small number of fibrin filaments on platelet aggregates, among which erythrocytes and leukocytes linger. After the formation of a platelet thrombus, it is compacted and fixed in the damaged vessel due to the retraction of the blood clot. Retraction is carried out under the influence of thrombostenin of platelets due to the reduction of the actin-myosin complex of platelets. A platelet plug forms in general within 1 to 3 minutes from the moment of injury, and bleeding from small vessels stops.
In large vessels, a platelet thrombus cannot withstand high pressure and is washed out. Therefore, in large vessels, hemostasis can be carried out by forming a more durable fibrin thrombus, the formation of which requires enzymatic coagulation.
mechanism.
The main stages of vascular-platelet hemostasis.
The first stage is adhesion (sticking of platelets to the site of damage, for example, to the subendothelial layer). This is followed by platelet activation and degranulation (showing some of the substances secreted by platelets). At the last stage, platelet aggregation occurs (binding of activated platelets with platelets adhering to the site of injury).
Coagulation hemostasis
Blood coagulation is a chain enzymatic process in which the activation of coagulation factors and the formation of their complexes occur sequentially. The essence of blood coagulation is the transition of soluble blood protein fibrinogen into insoluble fibrin, resulting in the formation of a strong fibrin thrombus.

Diagram of blood coagulation.
Clotting factors are traditionally denoted by Roman numerals, and their active forms by the letter "a".
There are two independent coagulation mechanisms - internal, or contact, and external, dependent on tissue factor. They converge at the stage of factor X activation and lead to the formation of thrombin, which converts fibrinogen to fibrin. These reactions are inhibited by antithrombin III, which binds all coagulation factors related to serine proteases (with the exception of factor VII), as well as by the protein C-protein S system, which inactivates factors V and VIII.
VMK - high molecular weight kininogen;
TM - thrombomodulin;
PC - prekallikrein;
PL - phospholipids.
The process of blood coagulation is carried out in 3 successive phases.
First phase is the most complex and lengthy. During this phase, the formation of an active enzymatic complex, prothrombinase, which is an activator of prothrombin, occurs. Tissue and blood factors take part in the formation of this complex. As a result, tissue and blood prothrombinases are formed. The formation of tissue prothrombinase begins with the activation of tissue thromboplastin, which is formed when the walls of the vessel and surrounding tissues are damaged. Together with factor VII and calcium ions, it activates factor X. As a result of the interaction of activated factor X with factor V and with tissue or plasma phospholipids, tissue prothrombinase is formed. This process lasts 5 - 10 seconds.
The formation of blood prothrombinase begins with the activation of factor XII upon contact with the collagen fibers of damaged vessels. High molecular weight kininogen (f XV) and kallikrein (f XIV) are also involved in the activation and action of factor XII. Factor XII then activates factor XI, forming a complex with it. Active factor XI, together with factor IV, activates factor IX, which, in turn, activates factor VIII. Then factor X is activated, which forms a complex with factor V and calcium ions, which ends the formation of blood prothrombinase. Platelet factor 3 is also involved in this. This process lasts 5-10 minutes.
Second phase. The resulting prothrombinase adsorbs the inactive plasma enzyme prothrombin (factor II) and on its surface converts it into the active thrombin enzyme. Factors IV, V, X and platelet factors 1 and 2 take part in this process. The second phase - the formation of thrombin - proceeds in 2-5 s.
Third phase. In this phase, the soluble blood protein fibrinogen is converted into insoluble fibrin, which forms the basis of a thrombus. Initially, under the influence of thrombin, the formation of fibrin monomer occurs. Then, with the participation of calcium ions, a soluble fibrin polymer (fibrin “S”, soluble) is formed. Under the influence of fibrin-stabilizing factor XIII, an insoluble fibrin-polymer (fibrin “I”, insoluble), resistant to fibrinolysis, is formed. In fibrin filaments, blood cells, in particular erythrocytes, are deposited, and a blood clot, or thrombus, is formed, which clogs the wound.
After the formation of a clot, the process of retraction begins, i.e. compaction and fixation of the thrombus in the damaged vessel. This occurs with the help of the platelet contractile protein thrombostenin and calcium ions. After 2 - 3 hours, the clot shrinks to 25 - 50% of its original volume and the whey is squeezed out, i.e. fibrinogen-free plasma. Due to retraction, the thrombus becomes more dense and tightens the edges of the wound.
fibrinolysis
Fibrinolysis is the process of splitting the fibrin clot, as a result of which the vessel lumen is restored. Fibrinolysis begins simultaneously with clot retraction, but proceeds more slowly. This is also an enzymatic process, which is carried out under the influence of plasmin (fibrinolysin). Plasmin is in the blood plasma in an inactive state in the form of plasminogen. Under the influence of blood and tissue plasminogen activators, its activation occurs. Urokinase is a highly active tissue activator. Blood activators are in the blood in an inactive state and are activated by adrenaline, lysokinases. Plasmin splits fibrin into individual polypeptide chains, resulting in lysis (dissolution) of the fibrin clot,
If there are no conditions for fibrinolysis, then the organization of a thrombus is possible, i.e. replacement with connective tissue. Sometimes a blood clot can break away from where it formed and block a vessel elsewhere (an embolism).
Factor VII of blood clotting, or, as it is also called - proconvertin, is formed in the liver and depends on the presence of vitamin K in the body. Factor VII activates factor X of blood clotting. The active form of factor VII is formed after vascular injury when factor VII binds to factor III. This is one of the main reactions that ensure blood clotting. In addition to factor III, factor VII can also be activated by coagulation factors XIIa, IXa, Xa and IIa.
Genetic mutations in factor VII can lead to decreased blood clotting and reduced thrombus formation. For example, this happens if guanine is replaced at position 10976 by adenine, causing the amino acid arginine to give way to glutamine.
The norm of factor VII in the blood. Result interpretation (table)
A blood test for factor VII is performed in order to assess the likelihood of a patient having a myocardial infarction, as well as in order to understand the possible causes of spontaneous abortion.
Blood is taken from a vein, in the morning, on an empty stomach.
The norm of factor VII in the blood of ordinary people and pregnant women:

If factor VII is elevated, what does it mean?
No data.
If factor VII is low, what does it mean?
Factor VII deficiency may be hereditary. This disease was first described in 1951. Bleeding from small vessels are detected, as a rule, immediately after the birth of a child, they look like small hematomas, the development of gastric or umbilical bleeding. But even if this is not immediately noticed, congenital factor VII deficiency will definitely manifest itself in the first two years of a child's life. Bleeding in any injury or surgery becomes especially strong, in women, congenital factor VII deficiency manifests itself in the form of extremely heavy monthly bleeding. The likelihood of developing a hemorrhagic stroke is extremely high due to the danger of cerebral hemorrhage.
The disease generally resembles hemophilia. With it, the risk of hemorrhages in the joints also remains, but they do not happen so often and do not lead to the development of osteoarthritis.
The disease can be mild, moderate or severe. With a mild degree of hemorrhage from the vessels, they may not appear at all, and reduced blood clotting manifests itself only during injuries and operations.
Acquired hypoproconvetremia (this is what this pathology is called) is usually caused by liver disease or after treatment with indirect anticoagulants. Decreased levels of factor VII in the blood are usually observed in the following diseases:
- viral hepatitis,
- acute alcoholic hepatitis,
- cirrhosis of the liver,
- chronic persistent hepatitis.
Monitoring the activity of factor VII can monitor the onset of liver failure.