The child's temperature is 37 after. Asymptomatic fever in children. Fever in a newborn
- this is a temperature at the level of 37-37.5 ° C for a long time. At the same time, a person may completely lack symptoms of any disease, and malaise may appear. We are talking about subfebrile temperature not when isolated cases of fever are recorded: this may be due to the individual characteristics of the body and the factors described above, but if subfebrile temperature is recorded in the temperature curve with measurements taken over many days in a row.
A true temperature increase is considered to be a temperature above 38.3 degrees.. Such a temperature is accompanied by very specific symptoms that correspond to a very specific disease. But prolonged low-grade fever is often the only sign to find out the cause of which you will have to run around the doctors.
The normal temperature of the human body is recognized as a temperature of 36.6 ° C, although for many, 37 ° C is fixed as a normal temperature. It is this temperature that is observed in a healthy organism: child or adult, male or female - it does not matter. This is not a stable static unchanging temperature, during the day it fluctuates in both directions depending on overheating, hypothermia, stress, time of day and biological rhythms. Therefore, temperatures from 35.5 to 37.4 ° C are considered the normal range.
Body temperature is regulated by the endocrine glands - the thyroid gland and the hypothalamus.. The receptors of the nerve cells of the hypothalamus respond to body temperature by changing the secretion of TSH, which regulates the activity of the thyroid gland. Thyroid hormones T3 and T4 regulate the intensity of metabolism, on which the temperature depends. In women, the hormone estradiol is involved in temperature regulation. With an increase in its level, the basal temperature decreases - this process depends on the menstrual cycle. In women, body temperature changes by 0.3-0.5 °C during the menstrual cycle. The highest rates of up to 38 degrees are observed between 15 and 25 days of a standard menstrual cycle of 28 days.
In addition to the hormonal background, temperature indicators are slightly affected by:
- physical exercise;
- food intake;
- in children: strong prolonged crying and active games;
- time of day: in the morning the temperature is usually lower (the lowest temperature is observed between 4-6 am), and in the evening it reaches a maximum (from 18 to 24 am - the period of max temperature);
- the temperature drops in the elderly.
Physiological fluctuations in thermometry during the day within 0.5-1 degrees are considered the norm.
Subfebrile condition does not belong to the normal state of the body and therefore the main question that is posed to the doctor is to identify the causes of the pathology. If the patient has recently been ill and treated for a long time, it is believed that the increase in temperature is associated with the recovery process. If there was nothing like that, then you have to look for the dysfunction that caused this symptom. For a more accurate detection of pathology, it is recommended to draw up a temperature curve, an analysis of well-being, and laboratory diagnostics.
Diseases that are characterized by subfebrile condition
Infectious causes of diseases
Infections are the most common cause of subfebrile condition. With the prolonged existence of the disease, the symptoms are usually erased and only subfebrile condition remains. The main causes of infectious subfebrile condition are:
- ENT diseases - sinusitis, tonsillitis, otitis media, pharyngitis, etc.
- Dental diseases and carious teeth including.
- Gastrointestinal diseases - gastritis, pancreatitis, colitis, cholecystitis, etc.
- Diseases of the urinary tract - pyelonephritis, cystitis, urethritis, etc.
- Diseases of the genital organs - inflammation of the appendages and prostatitis.
- Abscesses from injections.
- Non-healing ulcers in diabetic patients.
Autoimmune diseases
In autoimmune diseases, the body's immune system begins to attack its own cells, which causes chronic inflammation with periods of exacerbation. For this reason, body temperature also changes. The most common autoimmune pathologies:
- rheumatoid arthritis;
- systemic lupus erythematosus;
- Hashimoto's thyroiditis;
- Crohn's disease;
- diffuse toxic goiter.
To detect autoimmune diseases, tests for ESR, C-reactive protein, rheumatoid factor, and some other examinations are prescribed.
Oncological diseases
In malignant tumors, subfebrile condition can be an early manifestation of the disease, 6 to 8 months ahead of its symptoms. In the development of subfebrile condition, the formation of immune complexes that trigger an immune response plays a role. However, an early rise in temperature is associated with the onset of production of a specific protein by the tumor tissue. This protein is found in blood, urine, and tumor tissue. If the tumor has not yet manifested itself in any way, the combination of subfebrile condition with specific changes in the blood has a diagnostic value. Often subfebrile condition accompanies chronic myeloid leukemia, lymphocytic leukemia, lymphoma, lymphosarcoma.
Other diseases
Can cause subfebrile condition and other diseases:
- autonomic dysfunction: disruption of the heart and cardiovascular system;
- dysfunction of the endocrine glands: hyperthyroidism and thyrotoxicosis (ultrasound of the thyroid gland and a blood test for hormones T3, T4, TSH, antibodies to TSH are detected);
- hormonal disorders;
- latent infection: Epstein-Barr virus, cytomegalovirus infection, herpetic infection;
- HIV infection (detected by ELISA and PCR);
- helminthiasis (detected by analysis of feces for worm eggs);
- toxoplasmosis (identified by ELISA);
- brucellosis (detected by PCR);
- tuberculosis (detected by Mantoux tests and fluorography);
- hepatitis (identified by ELISA and PCR);
- Iron-deficiency anemia;
- allergic reactions;
- thermoneurosis.
For infectious subfebrile condition are characteristic:
- decrease in temperature under the action of an antipyretic;
- poor temperature tolerance;
- daily physiological fluctuations in temperature.
For non-infectious subfebrile condition are characteristic:
- imperceptible flow;
- lack of response to antipyretic;
- no diurnal changes.
Safe subfebrile condition
- Subfebrile temperature is completely safe during pregnancy, menopause and breastfeeding, which is simply a symptom of hormonal changes.
- Up to two months and even six months, a temperature tail can persist after suffering infectious diseases.
- Neurosis and stress may well provide a rise in temperature in the evenings. In this case, subfebrile condition will be accompanied by a feeling of chronic fatigue and general weakness.
Psychogenic subfebrile condition
Subfebrile condition, like any other processes in the body, is influenced by the psyche. With stress and neurosis, metabolic processes are primarily disturbed. Therefore, women often have unmotivated subfebrile fever. Stress and neuroses provoke an increase in temperature, and also excessive suggestibility (for example, about a disease) can affect the actual increase in temperature. In young women of the asthenic type, prone to frequent headaches and VVD, hyperthermia is accompanied by insomnia, weakness, shortness of breath, pain in the chest and abdomen.
To diagnose the condition, tests are prescribed to assess psychological stability:
- tests to detect panic attacks;
- scale of depression and anxiety;
- Beck scale;
- scale of emotional excitability,
- Toronto alexithymic scale.
According to the results of the tests, the patient is given a referral to a psychotherapist.
Medicinal subfebrile condition
Prolonged use of certain drugs can also cause subfebrile fever: adrenaline, ephedrine, atropine, antidepressants, antihistamines, antipsychotics, some antibiotics (ampicillin, penicillin, isoniazid, lincomycin), chemotherapy, narcotic painkillers, thyroxine preparations. Cancellation of therapy also relieves obsessive subfebrile condition.
Subfebrile condition in children
Of course, any parent will start to worry if their child has a fever every day in the evening. And rightly so, because in children, fever in some cases is the only symptom of the disease. The norm for subfebrile condition in children is:
- age up to a year (reaction to the BCG vaccine or unsteady processes of thermoregulation);
- the period of teething, when fever can be observed for several months;
- in children from 8 to 14 years old, due to critical growth phases.
About prolonged subfebrile condition, which occurs due to a violation of thermoregulation, they say if 37.0–38.0 ° in a child lasts more than 2 weeks, and the child at the same time:
- does not lose weight;
- examination shows the absence of diseases;
- all analyzes are normal;
- pulse rate is normal;
- temperature is not reduced by antibiotics;
- temperature is not reduced by antipyretics.
Often in children, the endocrine system is to blame for the increase in temperature. It often happens that in children with fever, the functionality of the adrenal cortex is impaired, and the immune system is weakened. If you draw a psychological portrait of children who have fever for no reason, then you get a portrait of an uncommunicative, suspicious, withdrawn, easily irritated child, whom any event can unsettle.
Treatment and the right lifestyle bring children's heat transfer back to normal. As a rule, after 15 years, few people have this temperature. Parents should organize the correct daily routine for the child. Children suffering from subfebrile condition should get enough sleep, walk and sit at the computer less often. Well trains thermoregulatory mechanisms hardening.
In older children, subfebrile temperature accompanies such frequent diseases as adenoiditis, helminthiasis, and allergic reactions. But subfebrile condition can also indicate the development of more dangerous diseases: cancer, tuberculosis, asthma, blood diseases.
Therefore, you should definitely consult a doctor if the child has a temperature of 37-38 ° C for more than three weeks. To diagnose and find out the causes of subfebrile condition, the following studies will be assigned:
- blood biochemistry;
- OAM, study of daily urine;
- feces on worm eggs;
- radiography of the sinuses;
- radiography of the lungs;
- electrocardiography;
- tuberculin tests;
- Ultrasound of internal organs.
If deviations are found in the analyzes, this will be the reason for referring narrow specialists for consultations.
How to measure the temperature in children
The temperature in children should not be measured immediately after waking up, after dinner, active physical activity, in an agitated state. At this time, the temperature may rise for physiological reasons. If the child is sleeping, resting or hungry, the temperature may drop.
When measuring temperature, you need to wipe the armpit dry and hold the thermometer for at least 10 minutes. Change thermometers periodically.
How to deal with subfebrile condition
To begin with, subfebrile condition should be diagnosed, because not every temperature increase in the specified range is precisely subfebrile condition. The conclusion about subfebrile condition is made on the basis of the analysis of the temperature curve, for the preparation of which temperature measurements are used 2 times a day at the same time - in the morning and in the evening. The measurements are carried out within three weeks, the results of the measurements are analyzed by the attending physician.
If the doctor diagnoses subfebrile condition, the patient will have to visit the following narrow specialists:
- otolaryngologist;
- cardiologist;
- infectiologist;
- phthisiatrician;
- endocrinologist;
- dentist
- oncologist.
Tests that will need to be passed to detect latent current diseases:
- UAC and OAM;
- blood biochemistry;
- cumulative urine samples and examination of daily urine;
- feces on worm eggs;
- blood for HIV;
- blood for hepatitis B and C;
- blood on RW;
- radiography of the sinuses;
- radiography of the lungs;
- otolaryngoscopy;
- tuberculin tests;
- blood for hormones;
- Ultrasound of internal organs.
Identification of deviations in any analysis becomes the reason for the appointment of a more in-depth examination.
Prevention measures
If the pathology in the body is not detected, you should pay close attention to the health of your body. To gradually bring thermoregulatory processes back to normal, you need:
- timely treat all foci of infection and emerging diseases;
- avoid stress;
- minimize the number of bad habits;
- observe the daily routine;
- get enough sleep in accordance with the needs of your body;
- exercise regularly;
- harden;
- walk more outdoors.
All these methods contribute to strengthening the immune system, training heat transfer processes.
A temperature of 37 in young children causes parental anxiety. On the one hand, this is not a fever when you urgently need to bring down high performance. On the other hand, subfebrile body temperature (37.1-37.4 ºС) may indicate the inability of the child's body to resist the disease in full force. Before giving medicine or rushing to the doctor, you should make sure that the readings are measured correctly.
Subfebrile temperature may be a sign of the body's inability to resist the disease.Temperature measurement rules
When the temperature rise is not accompanied by cough, runny nose, indigestion, overheating and other symptoms, you should make sure that it is measured correctly. No matter how accurate the thermometer is, there are exceptions that can change the indicators upwards:
- Crying and screaming can overestimate normal performance. Before measuring, you should calm the baby, and only then put a thermometer.
- After excitement, stress, a hot bath, physical activity, outdoor games, a long stay in a stuffy room, the data may be distorted. Measurements should be taken 30 minutes after returning to a normal calm state.
- Humidity distorts the readings, so before you put a thermometer, you should make sure that the baby's armpit is dry.
- The highest values are observed in the evening (they reach 37.5 ºС). In the morning hours, the parameters are the lowest. To obtain accurate information, measurements should be taken during the day, at the same hour.
At the first measurement, it may turn out that the temperature is slightly elevated. In this case, it is worth eliminating the above factors and checking the accuracy of the device. Electronic thermometers can show incorrect data, so you should double-check the measurements with a mercury thermometer (more in the article:). It is useful to confirm the accuracy of an electronic thermometer by measuring the readings of one of the older household members.

 The most reliable are the indicators of a conventional mercury thermometer
The most reliable are the indicators of a conventional mercury thermometer Can subfebrile temperature be considered normal?
When the accuracy of the measurements has been confirmed, teething and recent vaccination should be excluded. These factors allow an increase in values to 37.2-37.5 ºС and require waiting tactics. Also, subfebrile indicators may indicate imperfect thermoregulation, which does not require treatment.
Sea temperature without symptoms
Parents often travel with babies to the sea. Air, sun and water in moderation are good for the baby, but sometimes he gets a fever. The reason for this is:
- Acclimatization after two days of stay at the resort. A slight increase is natural, it indicates the adaptation of the body to new conditions, accompanied by lethargy and capriciousness.
- Food poisoning, in which the temperature reaches 38 degrees, there is indigestion and vomiting. It usually resolves within three days, but requires a doctor's examination.
- Sunny, heat stroke, which are accompanied by increased heart rate and heart rate, vomiting, headache (more in the article:). This condition requires urgent medical attention.

 During the child's stay at sea, the temperature may rise due to acclimatization (we recommend reading:)
During the child's stay at sea, the temperature may rise due to acclimatization (we recommend reading:) Why does the baby have a temperature of 37º?
With indications of 37.1 ºС in a 3-month-old child, it is important to focus on the condition of the baby. When he is active, eating and sleeping well, there is no reason to worry. In the first month of life, 37º C in a baby is considered the norm. Doctors distinguish transient hyperemia - a condition when, in the first hours of life, the temperature of a newborn rises to 38 ºС, then drops to 36.5 ºС and again rises slightly to 37.2 ºС. They explain subfebrile indicators by physiology:
- Newborns. 37.1 ºС in newborns is a variant of the norm. Most often, such indications are found in premature babies. Formation of thermoregulation can last up to a year.
- First 4 weeks. A variant of the norm is a temperature of 37.1-37.5 ºС per month in crumbs after vaccination against viral hepatitis. Another reason is the continued formation of thermoregulation.
- 2 months. In a 2-month-old baby, subfebrile indicators are noted after vaccination against pneumococcal infection or due to the continuation of the age-related formation of body temperature.
- 3-4 months. During this period, the crumbs are vaccinated against tetanus, whooping cough, polio, pneumococcal infection. After vaccination, within 3-5 days, the baby's temperature may rise to subfebrile values. This is the norm, but it is important to carefully monitor the well-being of the baby.
- 5 months of age. At this time, mothers begin to feed babies and subfebrile temperature can be caused by a reaction to a certain product. This is confirmed when the child has a tummy ache, loose stools, and flatulence are observed.
- Six months. At six months, in many babies, an increase in temperature indicators is associated with teething. It can be kept up to 5 days. It is worth taking all measures so that the process of teeth coming out is painless. There are special gels for this, and when the baby is too restless, you can give an anesthetic.

 An increase in temperature to subfebrile values \u200b\u200bcan be observed after routine vaccinations.
An increase in temperature to subfebrile values \u200b\u200bcan be observed after routine vaccinations. Overheating of the baby
In many cases, the cause of a fever in a child is overheating. The baby does not have developed sweat glands, through which sweat is released during the heat. Overheating under a layer of warm clothes, he does not sweat (see also:). A caring mother sees this and thinks that the baby is cold, wraps him up even more.
Babies tolerate overheating worse than cold. The face turns red, the heat rises, prickly heat may occur. In such a situation, you should lower the temperature in the nursery to 22 ° C, moisten the room. It is important to urgently change the baby into light cotton clothes, attach to the chest or give water from a bottle. Gradually, the fever will go away without medication.
Protein complementary foods
Mom's first protein complementary foods are introduced at 6-8 months. When the daily diet contains a lot of protein foods (egg, cottage cheese, mashed potatoes) and little ordinary water, a protein fever may occur in the crumbs. It is accompanied by an increase in temperature to 37.5 ° C and above, a sharp decrease in the frequency of urination. Sometimes a large fontanel may sink. The child drinks greedily, but does not give the impression of being sick. In this case, it is important to water the baby often, then the symptoms of fever will gradually go away.
Dysbacteriosis
Violation of the intestinal microflora also causes an increase in temperature in an infant. Beneficial microbes in the gut die, giving way to harmful ones. The toxins released by them enter the bloodstream and cause fever. It is accompanied by poor appetite, unstable stool. In this case, it is important to give an analysis that confirms dysbacteriosis and undergo treatment with a doctor.
What does a temperature of 37 and additional symptoms indicate?
Usually, up to six months, babies rarely get sick with viral and bacterial infections. Contact with society is limited, but even in this case, the disease can be picked up at the clinic at a scheduled appointment or infected from one of the family members. After the 6th month of life, the risk of getting sick increases. Complementary foods, contacts with other children begin, which increases the likelihood of getting rubella, chickenpox, SARS. Particular attention should be paid to the condition when the temperature increase in the baby is accompanied by the following symptoms:
- lethargy, weakness - the beginning of an infectious disease;
- runny nose - allergies, colds;
- cough - a symptom of allergies, colds, incipient bronchitis, pneumonia;
- hoarse voice - tonsillitis, measles, laryngitis, influenza, asthma, pneumonia, measles, diphtheria;
- vomiting - food poisoning, gastrointestinal diseases, encephalitis, meningitis;
- diarrhea is an intestinal infection;
- headache - SARS, influenza, sinusitis, thermoneurosis, intoxication;
- abdominal pain - tonsillitis, measles, acute respiratory infections, whooping cough, food poisoning, appendicitis, foreign body in the stomach.
Infectious diseases of the baby are fraught with complications - pneumonia, bronchitis, sinusitis, tonsillitis. It is important for mom not to miss their beginning, to show the child to the doctor in time and get appointments. Subfebrile indicators can last a long time after taking antibiotics and a serious illness.
In this case, treatment is not required, but the situation must be kept under control. Repeated runny nose, cough and other symptoms indicate a relapse or the addition of a new infection. It is important to consult a pediatrician to prevent complications and find out why the temperature rises.
What to do if the temperature is 37 for more than a week?
An increase in temperature from time to time usually indicates overheating or measurement errors. In this case, it is important for parents to monitor the condition of the crumbs, to record changes in the diary. When the baby is active and nothing bothers him, no treatment is required.
If subfebrile indicators last more than a week, you should not rush with antipyretics. In any situation, even if the baby feels good, it is important to take the following measures:
- Identify what worries the baby - pain, runny nose, cough and more.
- Observe the drinking regime - elevated temperature disrupts the water-salt metabolism, provokes dehydration. You should often apply crumbs to the chest or drink water from a bottle. Grown up children can be offered cranberry juice, dried fruit compotes.
- In case of a sharp deterioration in well-being (wheezing, vomiting, convulsions, difficulty breathing, fever against the background of antipyretics), call an ambulance, otherwise, make an appointment with a doctor.
- Create a comfortable microclimate in the baby's room - moderate humidity, air temperature 21 + 22 ° C. In a dry, hot room, ARVI in infants is often fraught with complications in the form of bronchitis, otitis media, and pneumonia.
- Dress your baby in light clothing if he is not chilly. A thin knitted blouse and sliders are ideal. During sleep, the crumbs can be covered with a thin fleece blanket.
Often a child has a temperature of 37 and above after vaccination. It is important for mom to monitor the condition of the crumbs, and report any changes in his health to the pediatrician. Antipyretics in this case should be given deliberately, since vaccination can cause hypothermia. The action of paracetamol or ibuprofen will only aggravate the situation.

 At elevated temperatures, the child's body loses a lot of fluid, so you need to regularly replenish its supply (see also:)
At elevated temperatures, the child's body loses a lot of fluid, so you need to regularly replenish its supply (see also:) When and how to bring down the temperature?
If the baby's temperature has not reached 37.5 ° C and passes without symptoms, it is not recommended to knock it down (this can weaken the already imperfect immunity of the child).
At values of 37.7-38.2 ° C, it is worth using safe physical methods (compresses, wiping with water). If the thermometer readings have stepped over 38.4 ° C (fever), you need to connect drugs with ibuprofen or paracetamol.
Assistant to young mothers in raising healthy babies, Dr. Evgeny Komarovsky, believes that a temporary increase in temperature does not pose a threat. However, in order not to scold yourself later for slowness and sluggishness, parents should show the baby to a competent doctor.
Dangers of subfebrile temperature
At a subfebrile temperature, an infant may not be disturbed by anything, but apparent well-being can be deceptive. A prolonged, even a slight increase in temperature can signal hidden problems in the child's body - anemia, helminthic invasion, infections, brain disease. They can only be detected with a thorough medical examination. When no pathologies have been identified, attention should be paid to strengthening the defenses of the baby's body.
Preventive measures
A prolonged increase in body temperature leads to chronic stress of the body. When doctors convince that this is a variant of the norm, you should still try to bring the indicators to 36.6. Prevention of fever is hardening, the correct daily routine, regular walks, the identification and treatment of foci of infectious diseases. These measures strengthen the immune system, help to establish thermoregulation and cope with low-grade fever.
Update: October 2018
Subfebrile condition - rise in temperature from 37 to 37.9 degrees Celsius. A body temperature above 38 degrees is usually accompanied by very specific symptoms that any doctor can tie to a specific disease. But prolonged subfebrile condition often remains the only sign that makes the patient visit many specialists and take many tests.
Why does the body need subfebrile temperature?
Man is a warm-blooded creature, so we are able to maintain a more or less stable body temperature throughout our lives. Fluctuations up to 1 degree can occur during stress, after eating, during sleep, and also depending on the woman's menstrual cycle. When exposed to certain factors, a protective reaction of the body may occur - fever. Even subfebrile temperature numbers can speed up the metabolism and make it impossible for many harmful microbes to multiply. In addition, a temperature rise can indicate bodily or psychological ill health.
Normal human body temperature
The average temperature when measured in the armpit is 36.6 degrees Celsius. But for different people, this value can be individual. For some, the thermometer rarely shows a value greater than 36.2, and someone constantly lives with numbers of 37-37.2 degrees. However, in most cases, subfebrile temperature indicates a sluggish inflammatory process in the body, so you should find out the cause of subfibrillation and find the focus of inflammation.
The upper limit of normal human temperature is 37.0, everything that is higher can be considered as a sluggish inflammatory process and requires careful diagnosis. In a child under one year old, a temperature of 37.0-37.3 is normal due to an unsteady thermoregulation system.
However, the state in which the measurement takes place must be taken into account. If, for example, you measure the temperature of a person overheated in the sun or dressed in a woolen sweater, or if the patient has hyperthyroidism, a violation of thermoregulation, this should be taken into account.
How to measure temperature correctly?
There are several areas of the body where temperature is usually taken. The most common are the rectum and armpits. In the rectum, it is customary to measure the temperature in children, such data are more accurate, although some babies actively resist this procedure. And subfebrile condition in infants is not at all a reason to torment a child with rectal measurements. The classic version of thermometry in adults is in the armpit.
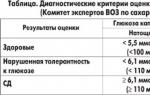
Temperature standards:
- armpit: 34.7C - 37.0C
- rectum: 36.6C - 38.0C
- in the oral cavity: 35.5C - 37.5C
Causes of subfebrile condition
infectious causes
Infections are considered the most common cause of subfebrile temperature. So, the majority of banal SARS is accompanied by malaise, headache and joint pain, runny nose, cough and subfebrile condition. Some childhood infections (rubella, chickenpox) are not severe, with a low temperature. In all these cases, there are clear signs of the disease.
With the prolonged existence of a focus of inflammation, all symptoms are erased or become habitual. Therefore, the only sign of trouble remains a long subfebrile condition. In such cases, finding the source of the infection can be difficult.
Foci of infection, most often causing a prolonged rise in temperature:
- ENT diseases - pharyngitis, etc.
- Dental - carious teeth
- Diseases of the gastrointestinal tract -,), etc.
- Inflammation of the urinary tract - pyelonephritis, urethritis, cystitis, etc.
- Inflammatory diseases of the female and male genital organs -,.
- Abscesses at injection sites
- Non-healing ulcers in the elderly and sick
To detect a sluggish infection, the doctor will prescribe:
- General analysis of blood and urine. Deviations in some indicators may indicate an inflammatory process in the body. For example, a change in the leukocyte formula and.
- Inspection by narrow specialists: ENT doctor, gastroenterologist, surgeon, dentist, gynecologist
- Additional Methods: CT scan, x-ray, ultrasound if inflammation is suspected in a particular organ.
If the source of inflammation is found, then it will take some time to heal, since chronic infections are less well treated.
Rarely diagnosed infections
Toxoplasmosis
 A very common infection, but clinical manifestations are rare (see). Almost all cat lovers are infected with it. In addition, you can get infected by eating undercooked meat.
A very common infection, but clinical manifestations are rare (see). Almost all cat lovers are infected with it. In addition, you can get infected by eating undercooked meat.
Clinically significant is only (due to the risk of pathology in the fetus) and HIV-infected (due to the severity of the course). In a healthy person, toxoplasmosis is present as a carrier, sometimes causing low-grade fever and eye damage.
The infection does not require treatment (except in severe cases). It is diagnosed with the help of ELISA (determination of antibodies), which is especially important when planning a pregnancy.
Brucellosis
This is a disease that is often forgotten when looking for the causes of subfebrile condition. It is mainly found in farmers and veterinarians in contact with farm animals (see). The symptoms of the disease are varied:
- fever
- joint, muscle and headache
- hearing and vision loss
- confusion
This disease is not life-threatening, but can lead to a permanent change in the psyche and motor sphere. For diagnosis, PCR is used, which with high accuracy determines the source of the disease in the blood. Brucellosis is treated with antibiotics.
When infected with helminths in the organs, a sluggish inflammatory process can occur for a long time. And often subfebrile condition is the only symptom of helminthic invasion (see). Therefore, with prolonged fever, especially combined with weight loss and indigestion, you can take tests:
- Complete blood count for - cells growing during an allergic reaction to helminths
- ESR is a sign of inflammation in the body
- analysis of feces for worm eggs (the most common in a particular region, see,)
Treatment of helminthic invasion is carried out with special preparations (see). Sometimes one dose is enough for a complete recovery.
Tuberculosis
There is an erroneous opinion that tuberculosis is a disease of the past, it is now found only in places of deprivation of liberty and only asocial persons are ill. In fact, the number of TB patients is not decreasing, but even growing. Everyone is at risk of getting sick, especially small children, medical workers, students in hostels, soldiers in the barracks. In general, the tubercle bacillus loves places with a large crowd of people constantly living under the same roof. 
Risk factors:
- insufficient and unbalanced nutrition
- chronic lung diseases
- diabetes
- living with a person who is a source of tuberculosis
- tuberculosis in the past
Tuberculosis is a bacterial infection that mainly affects the lungs. In this case, the annual Mantoux test in children and fluorography in adults allows you to suspect and cure the disease in time.
If other organs are involved in the process, then with a “clean” x-ray of the lungs, it can be extremely difficult to find the cause of the ailment, since the tuberculous lesion of the internal organs is perfectly disguised as non-specific inflammatory processes. Until now, the diagnosis of extrapulmonary forms is extremely difficult, and also when differentiating the diagnosis, this infection is often “forgotten”.
Signs of tuberculosis:
Are common:
|
Urinary system:
|
Pulmonary forms:
|
Genital tuberculosis:
|
Bone and articular forms:
|
Skin and ocular forms:
|
To identify the disease, it is necessary to undergo a chest examination (fluorography), conduct tuberculin tests (Mantoux), Diaskintest; if necessary - computed tomography of internal organs, radiography of the kidneys, etc.
Diagnosis of tuberculosis:
Mantoux test - intradermal injection of a special protein from the destroyed shell of bacteria (tuberculin). This protein cannot cause disease, but in response to it, a skin reaction occurs, according to which the test is evaluated. The Mantoux test for most children is carried out 1 time per year.
- In children under 5 years of age, the reaction should be positive (papule from 5 to 15 mm). If the reaction is negative, then the child has an innate immunity to the disease or he has received a poor-quality BCG vaccination (or not done at all). If the papule is more than 15 mm, an additional examination is necessary.
- If the reaction has increased sharply compared to the previous one (more than 6 mm compared to the previous one), then this is considered a turn. That is, the child was infected with Mycobacterium tuberculosis. These children are more likely to get this infection. Therefore, after an additional examination, the child is prescribed prophylactic doses of anti-tuberculosis drugs.
It is important to know:
- the injection site can be wetted, this does not affect the size of the papule.
- you can eat sweet and citrus fruits - this does not affect the size of the papule if the child does not suffer from a severe allergy to these products.
- Mantoux test is not capable of causing tuberculosis
- Diaskintest is a test similar to Mantoux, but giving a greater percentage of accuracy. The reaction to intradermal administration is also checked after 72 hours. The results of the test are not affected by BCG vaccination. Therefore, a positive result of the test is almost 100% infection with Mycobacterium tuberculosis and the development of the disease. However, when infected with a bovine type of mycobacterium (unboiled milk, contact with a sick cow, cat, dog, etc.), as well as with a complication of BCG vaccination (extremely rare, but there are complications of the type of persistent or disseminated BCG - infection when the vaccine strain is "activated "in debilitated children), Diaskintest remains negative, and does not give a 100% exclusion of bovine tuberculosis or activation of BCG vaccination.
Tuberculosis treatment- long, hard to bear, but still vital. Without therapy, tuberculosis slowly incapacitates a person and leads to death. A timely BCG vaccination protects young children from severe lethal forms of the disease, but unfortunately, it does not protect either children or adults from the disease during prolonged contact with a patient with an active form. Modern drugs make it possible to cure foci of infection, but in recent decades, the number of drug-resistant forms that are difficult to treat has been growing.
HIV infection
The human immunodeficiency virus attacks the body's defense system, making it defenseless against any, even the mildest infection. Virus infection occurs in the following ways (see):
- with unprotected sex
- when injected with contaminated syringes
- with blood transfusions
- during manipulations in the office of a dentist, cosmetologist
- from mother to fetus
Since a large number of viral particles are required for infection, it is impossible to get HIV infection from coughing, sneezing or touching a sick person.
Symptoms of HIV infection:
During the incubation period (1-6 months from infection) there are no subjective signs.
In the acute period, complaints may appear:
- Subfebrile condition or high temperature
- Enlarged lymph nodes
- Rash of a different nature
- Headache, nausea and vomiting
- Pain in muscles and joints
A latent period without obvious symptoms, but with active reproduction of the virus in the blood. Can last up to 20 years.
AIDS-associated complex (diseases that often occur and are severe in the development of AIDS):
- (thrush in mouth)
- Leukoplakia in the mouth (mucosal changes)
- Herpes with multiple recurrences
- Pneumocystis pneumonia (not responding to standard antibiotics)
- Tuberculosis
- Subfebrile condition, weight loss
- Inflammation of the parotid glands
- Dysplasia and
- Kaposi's sarcoma
- Toxoplasmosis of the brain
- Other inflammatory diseases
Diagnosis of HIV infection:
- ELISA (enzymatic immunoassay). This is the first stage of the survey, which is carried out at the request of many employers. With the above symptoms, this method alone is not enough. In most infected patients, antibodies to the virus appear after 3 months, in some, a positive result appears only after 6-9 months. Therefore, it is recommended to conduct a study twice: after 3 and 6 months from a possible infection.
- PCR (polymerase chain reaction). A very effective method that allows you to detect viral particles as early as 2 weeks after infection.
- methods for determining viral load and immune suppression. Additional methods used in a confirmed diagnosis.
With a definitive diagnosis of HIV infection, antiretroviral treatment should be initiated. It will allow you to delay the onset of AIDS as much as possible, alleviate existing symptoms and significantly prolong the life of the patient.
Viral hepatitis B and C
One of the causes of intoxication and, as a result, subfebrile temperature, are viral hepatitis. These diseases begin in different ways: some acutely, with pain in the hypochondrium, jaundice, high fever. Some practically do not feel the onset of the disease (see)
Signs of sluggish viral hepatitis:
- malaise, weakness
- subfebrile condition, sweating
- discomfort in the liver after eating
- slight, almost imperceptible jaundice (see.
- joint and muscle pain
Since a large percentage of viral hepatitis becomes chronic, subfebrile condition can return with each exacerbation.
Ways of transmission of viral hepatitis:
- sexual contact
- medical instruments
- blood transfusions
- tools in manicure and dental offices
- syringe needles
- from mother to fetus
Diagnosis of viral hepatitis:
- PCR - a method with high accuracy, determines the particles of viruses in the blood
- ELISA is a method that allows you to detect antibodies to various components of the virus. With its help, you can determine the carriage, the active form of the disease, the risks of infection of the fetus. It is also possible to distinguish between acute and chronic hepatitis.
Treatment of acute hepatitis of a viral nature is not carried out. Associated complications are usually treated. Treatment of chronic hepatitis during the period of exacerbation is carried out with special antiviral drugs, choleretic agents. A chronic process in the liver can lead to cancer, so all patients with hepatitis should be regularly examined by a specialist.
Tumors
With the development of a malignant tumor in the body, all organ systems begin to work differently. The metabolism also changes. As a result, paraneoplastic syndromes occur, including subfebrile condition. A tumor can be suspected after the exclusion of more obvious causes (infection, anemia). A malignant neoplasm during decay releases pyrogens into the blood - substances that increase the temperature. Often, infections are exacerbated against the background of the tumor, which also causes fever. 
Features of paraneoplastic syndromes:
- respond poorly to standard therapy for this symptom
- often recur
- decrease in the treatment of the underlying disease (tumor)
Frequent paraneoplastic syndromes:
Fever, difficult to treat with antipyretic and anti-inflammatory drugs.
Skin manifestations:
- Black acanthosis (for cancer of the digestive system, breast and ovaries)
- Erythema Darya (with and)
- without rash and obvious reasons
Endocrine signs: 
- Cushing's syndrome (excessive production of ACTH - adrenal hormone) - with cancer of the lung, pancreas, thyroid or
- Gynecomastia (breast enlargement in men)
- - with cancer of the lungs, digestive organs
Blood changes:
- Anemia (with tumors of different localization). Anemia itself also leads to prolonged subfebrile condition.
- Elevated ESR (over 30) for a long time
It should be noted that not all cancer patients have obvious paraneoplastic syndromes. And not all of the above signs necessarily indicate a tumor. Therefore, when subfebrile condition of unclear etiology appears, especially in combination with other paraneoplastic signs, a thorough examination is necessary.
Thyroid disease
With increased work of the thyroid gland (), all metabolic processes are sharply accelerated. This immediately affects the body temperature. In those suffering from thyrotoxicosis, the thermometer rarely shows less than 37.2 degrees.
Signs of thyrotoxicosis:
- subfebrile condition
- irritability
- rapid pulse, high blood pressure
- liquid stool
- weight loss
- hair loss
To diagnose thyrotoxicosis, you need to do an ultrasound of the thyroid gland and donate blood for hormones: T3, T4, TSH and antibodies to TSH. According to the results of the tests, the doctor will prescribe the appropriate treatment.
Anemia - as an independent disease or a component of other diseases
Anemia is a decrease in hemoglobin levels. This condition occurs for various reasons, ranging from chronic bleeding (with hemorrhoids, for example), ending with iron malabsorption (in diseases of the gastrointestinal tract). It is iron deficiency that in most cases is the cause of this condition. Often anemia occurs in women with heavy menstruation and in vegetarians who have refused animal products.
The lower limits of the norm of hemoglobin:
- Men: 20 to 59 years old: 137 g/l, over 60 years old: 132 g/l
- Women: 122 g/l
In some cases, the hemoglobin level may be normal, but the iron content in the blood is sharply reduced. This condition is called latent iron deficiency.
Signs of anemia and latent iron deficiency:
- unmotivated subfebrile condition
- cold hands and feet
- loss of energy and decreased performance
- frequent headaches and dizziness
- bad hair and nails (see)
- daytime sleepiness
- aversion to meat products and a tendency to eat inedible
- itchy skin, dry skin
- stomatitis, glossitis (inflammation of the tongue)
- poor tolerance for stuffy rooms
- unstable stool, urinary incontinence
The more of the above signs, the higher the likelihood of iron deficiency in the body. The following tests are required to confirm the diagnosis:
- Blood test for hemoglobin
- ferritin level
- If necessary, examination of the digestive system
If iron deficiency is confirmed, then it is necessary to start treatment with ferrous iron preparations. These are Sorbifer, Tardiferon, Ferretab (see). All iron preparations should be taken together with ascorbic acid, for at least 3-4 months.
Autoimmune diseases
In autoimmune diseases, the body begins to attack itself. Immunity is tuned against the cells of certain organs and tissues, causing chronic inflammation with periods of exacerbation. Against this background, the body temperature also changes.
The most common autoimmune diseases:
- Rheumatoid arthritis
- (thyroid damage)
- Crohn's disease (bowel disease)
- Diffuse toxic goiter
To diagnose autoimmune conditions, the following tests are needed:
- Erythrocyte sedimentation rate (ESR) - an indicator, the increase of which indicates an inflammatory reaction
- C-reactive protein - a parameter in a biochemical blood test, indicates inflammation
- Rheumatoid factor (increased in rheumatoid arthritis, other autoimmune processes)
- LE cells (for diagnosing systemic lupus erythematosus)
- additional examination methods
With a proven diagnosis, treatment must begin. It includes hormonal agents, anti-inflammatory, immunosuppressants. Therapy allows you to control the disease and reduce the risk of exacerbations.
Residual effects after illness
All people at least once in their lives suffer - an acute respiratory viral infection. Often the main symptoms do not last longer than a week: cough, runny nose, high fever and headache. But subfebrile condition can persist for several months after the illness. There is no need to treat this condition, it will go away on its own. You can improve your health with dosed physical activity and walks in the fresh air (see).
Psychogenic causes
Subfebrile condition is a manifestation of an accelerated metabolism. It, like all processes in the body, is influenced by our psyche. With stress, anxiety and neurosis, it is the metabolic processes that are disturbed in the first place. Therefore, in people with a fine mental organization, especially in young women prone to hypochondria, unmotivated subfebrile fever is often observed. And the more actively temperature measurements take place, the worse a person feels. To diagnose this condition, you can take tests to assess psychological stability:
- Questionnaire for identification
- Hospital Depression and Anxiety Scale
- Beck scale
- Individual typological questionnaire
- Toronto alexithymic scale
- Scale of emotional excitability
Based on the results of these tests, you can draw conclusions and, if necessary, contact a psychotherapist (do not forget to take these results with you). Treatment of such a condition can be reduced to psychotherapy sessions and admission,. Often, all unpleasant symptoms go away when a person realizes the groundlessness of fears and stops measuring the temperature.
Medicinal subfebrile condition
Prolonged or active use of certain drugs can cause an increase in temperature to subfebrile numbers. These funds include:
- epinephrine, ephedrine, norepinephrine
- atropine, some antidepressants, antihistamines, and antiparkinsonian drugs
- antipsychotics
- antibiotics (penicillin, ampicillin, isoniazid, lincomycin)
- chemotherapy for tumors
- narcotic painkillers
- thyroxine (thyroid hormone) preparations
Cancellation or replacement of therapy eliminates unpleasant subfebrile condition.
Subfebrile condition in children
The causes of subfebrile temperature in a child are exactly the same as in adults. But parents should remember that a temperature of up to 37.3 degrees in a child under one year old is considered normal and does not require a search for reasons. Therefore, if the baby feels well, is active, cheerful and does not suffer from a lack of appetite, then subfebrile condition should not be treated. However, if a child older than a year has a long subfebrile condition, lack of appetite, weakness, the cause should be established.
How to find the cause of subfebrile condition?
To exclude dangerous and even fatal options, you need to be examined by specialists.
Examination algorithm at subfebrile temperature:
- Determination of the nature of the fever: infectious or non-infectious
- General blood analysis
- Analysis of feces for helminths
- : determination of c-reactive protein
- X-ray of the chest (to exclude tuberculosis, endocarditis, lung cancer)
- X-ray or CT scan of the sinuses (to rule out sinusitis)
- Ultrasound of the heart, digestive organs
- Bacteriological culture of urine (to rule out inflammation in the urinary system)
- Tests with tuberculin, diaskintest (to exclude tuberculosis)
Additionally:
- Using additional methods to exclude HIV, brucellosis, viral hepatitis, toxoplasmosis
- Consultation with a phthisiatrician for indeterminate tuberculin tests, night sweats, weight loss
- Consultation with an oncologist and hematologist (to rule out tumors and blood diseases)
- Rheumatologist's consultation
- Psychotherapist's consultation
- How to measure correctly?
- Norm
- Age features
- What to do?
- Diagnostics
- Prevention
One of the most controversial and alarming situations for parents is when a child has a temperature of 37 ° C, which in medicine is called subfebrile. Someone says that this is the norm that every person should have. Some consider this an indication that a small organism cannot fully resist the disease, which in itself is a very bad sign.
And doubts always begin: to go to the hospital or not? Give antipyretics or take a wait-and-see attitude? What if precious time is wasted? In such serious matters relating to the health of the baby, you need to understand in detail.
- Very often, a temperature of 37-37.3 ° C is explained by physical exertion that the child has just endured. It could be both sports, and household chores or outdoor games. Therefore, give him a thermometer only half an hour after active actions.
- The data may be inflated after crying or screaming, so first you need to wait until the baby calms down.
- Carry out thermometry during the day, preferably always at the same time. And keep in mind that in the morning the thermometer usually gives low readings, and in the evening the temperature can rise to 37-37.5 ° C.
- The armpit into which the thermometer is inserted must be completely dry, otherwise the humidity will distort the readings.
- Do not take oral measurements (through the mouth) if the child has just eaten or drunk hot liquid, breathes through the mouth, coughs heavily, or is short of breath.
- Data may be higher than normal after a hot bath, stress, fatigue, excitement, prolonged exposure to the sun or in a stuffy room.
So, if you see a mark of 37 ° C or a little higher on the thermometer, do not panic. First, check yourself with this memo: have you violated the rules of measurement.
In addition, very often errors are given out by electronic thermometers. Therefore, put it for someone else to check, or confirm the data obtained with an ordinary mercury thermometer.
Origin of name. The term "subfebrile" goes back to the Latin words "sub" - a little and "febris" - fever. That is, the literal translation is a little fever.
Norm
If the child has a temperature of 37 ° C, and there are no more symptoms with accurate measurements, this is also not a cause for alarm. In some situations, it is the norm:
- vaccination;
- teething;
- a temperature of 37 ° C in an infant is a sign of immature thermoregulation, which does not require treatment and will pass by itself;
- the introduction of protein complementary foods in too large quantities.
Asymptomatic subfebrile temperature in a child may be due to various circumstances, but in most cases it is the norm and does not require a visit to a doctor. You need to take a wait-and-see attitude.
It is quite another matter if the mark on the thermometer at 37 ° C is accompanied by a painful condition. Here it is already necessary to urgently find out the reasons and take appropriate measures.
through the pages of history. Galileo is considered the inventor of the first thermometer, although there is no description of the device in his own writings. However, his students testified that in 1597 the scientist made something like a thermobaroscope.
Causes and additional symptoms
The normal temperature of 37-37.5 ° C in a child is rare. Much more often this is a sign of some kind of pathology. The causes can be various diseases that can be identified even before visiting a doctor for certain symptoms.
The child has a temperature of 37 and ...
- …cough- bronchitis (at the beginning of the disease there will be a dry cough), colds, chronic tonsillitis, allergies, pneumonia, tuberculosis;
- …runny nose- colds, allergies;
- …vomit- food poisoning, intestinal infection, CNS pathology (encephalitis, meningitis), gastrointestinal diseases;
- …I have a stomachache- appendicitis, tonsillitis, whooping cough, acute respiratory infections, measles, intestinal infection, food poisoning, foreign body in the stomach;
- …diarrhea- intestinal infection, helminthic invasion;
- …headache- flu, SARS, sinusitis, meningitis, intoxication, thermoneurosis;
- ... hoarse voice- tonsillitis, influenza, asthma, laryngitis, pneumonia, tracheitis, measles, diphtheria;
- ... lethargy- the onset of infection, inflammation, the rehabilitation period after abdominal operations, helminthic invasion, oncology.
It also happens that after antibiotics and after illness, the temperature of 37 ° C lasts for quite a long time. Rates may remain elevated for up to several months. Treatment is not required, the condition resolves on its own without consequences.
But if in parallel with this there is a cough, runny nose, lethargy or other symptoms - most likely, a relapse of the disease was provoked, complications arose, or a new infection superimposed on the old one. In this case, you must consult a doctor.
This is interesting. When a subfebrile temperature lasts for several days and even weeks after a treated disease, doctors call this feature a “temperature tail”.
Age features
The question of why a child has a temperature of 37 ° C can also be answered by age-related physiology. This is especially true for the smallest - infants of the first year of life.
- Newborn
If the temperature is 37 ° C in a newborn child without any deviations in health, this is a variant of the norm, which indicates a thermoregulation system that has not yet been formed. Most often this happens with premature babies.
- Month
If a month-old child has a temperature of 37 ° C after being vaccinated against viral hepatitis ("A" or "B"), you should not worry - this is the norm. Another reason is the formation of a thermoregulation system, which can last up to a year.
- 2 months
Subfebrile indicators in a two-month-old child are a consequence of vaccination against pneumococcal infection or age-related development of body temperature.
- 3-4 months
The situation also changes little in a 3-4 month old child. Since this period is replete with vaccinations (for diphtheria, whooping cough, tetanus, polio, hemophilia and pneumococcal infections), the temperature can rise to 37 ° C after each vaccination, and this will be the norm.
- 5 months
Subfebrile indicators can be caused by the first feeding. If the baby has a temperature of 37 ° C and his stomach hurts due to constipation, colic, bloating, flatulence, the cause may be the unsuccessful introduction of protein foods into his diet.
- 6-7 months
The main reason for slightly inflated rates at this age is teething. Then the temperature of 37 ° C will be kept in the child constantly - for 5-7 days.
At a later age, this problem can be associated with only two factors: puberty and depression. If a child finds himself in an unfamiliar situation or experiences severe stress, his nervous system begins to regulate body temperature itself and raises it to subfebrile. Most often this happens during adolescence.
What do children need to normalize such an incomprehensible state?
Curious fact. Body temperature limits for human survival range from +20°C to +41°C.
What to do?
If subfebrile indicators are observed from time to time, most likely, the matter is in measurement errors, so nothing is required from parents other than calmness and observation.
Another thing is if a child has a temperature of 37 ° C for a week or more, regardless of whether it is accompanied by some additional symptoms or not. In this case, a number of measures should be taken.
- Identify the clinical picture - all deviations in the condition (cough, runny nose, diarrhea, rash, headache, etc.).
- With a sharp deterioration (severe vomiting, for example), call an ambulance. In other cases, just see a doctor.
- Many parents worry about what to give their child at 37°C: nothing but water. Plentiful warm drink will improve his condition, remove all products of intoxication from the body. No antipyretics!
- Bed rest is not required at all.
- Provide fresh air: ventilate the room, go out more often (to the question of whether it is possible for a child with a temperature of 37 ° C to walk).
- Limit your time at the computer (laptop, phone, TV).
- Provide a favorable psychological atmosphere, dispel fears, help overcome difficulties, and call for a confidential conversation.
- But the question of whether it is possible to bathe a child at a temperature of 37 ° C causes different opinions. Some doctors are categorically against large-scale water procedures in such a situation (shower, bath, bath). It is better to wait until the fever subsides, and until then limit yourself to washing and local rinsing.
- Establish proper nutrition.
- Make sure you get at least 8 hours of sleep.
So if a child has a fever for a week, be sure to make an appointment with a doctor to get diagnosed, to identify more accurately what is the cause of subfebrile condition, and to be treated if necessary.
This is interesting. The temperature regime of 35.8-37.3 ° C is a guarantee of the uninterrupted functioning of all internal organs.
Diagnostics
If a child has a temperature of 37 ° C for a long period, you first need to contact a pediatrician (therapist). Depending on additional symptoms, he may prescribe the following examinations:
- general and biochemical blood test;
- general urine analysis;
- Ultrasound of the abdominal cavity, pelvic organs, kidneys;
- echocardiography (ultrasound of the heart);
- chest x-ray;
- narrower blood tests to identify the hormonal profile, antibodies, tumor markers.
These are standard research methods. In more advanced and severe cases (when the temperature stays at 37 for a week or longer and is accompanied by various clinical manifestations and deterioration of the child's condition), a puncture of the cerebrospinal fluid, computed tomography, and magnetic resonance imaging may be required.
The doctor will prescribe tests gradually. The examination plan depends on the symptoms against the background of subfebrile fever. If there are none, the visit to the hospital will be limited to the passage of a routine medical examination.
Wow! There is a known case when a man was rescued, who was diagnosed with a body temperature of 13 ° C.
Prevention
Parents need to keep in mind that even if no diseases were detected in the child during the diagnosis and the doctor said that a constant temperature of 37 ° C for him is a variant of the norm, this does not mean at all that you need to calm down, fold your hands and do nothing do.
Such indicators for a long time are chronic and dangerous stress for the body. We must try to bring the child's body back to normal.
Preventive measures in this case will include:
- timely detection and treatment of foci of infections and various diseases;
- salvation from stress, favorable psychological atmosphere;
- refusal of bad habits (referring to adolescents);
- compliance with the daily routine;
- full sleep;
- regular exercise;
- hardening;
- daily outdoor walks.
These preventive methods will help strengthen the immunity of the child and train the processes of heat transfer. With the exact implementation of the recommendations, the children's body will quickly return to normal and cope with subfebrile condition.
A temperature of 37 without accompanying symptoms sometimes causes anxiety and anxiety in parents. There is an opinion that this is a dangerous indicator of a thermometer, and if at the same time the patient does not feel much discomfort, then it remains only to wait - whether the temperature rises higher, stays or drops. How to treat such an indicator of a thermometer from the point of view of medicine? First of all, you need to make sure that the thermometer is working. Despite the fact that modern medicine offers us several types of thermometers, but so far the mercury one shows the most accurately.
If you are convinced that the child really has a temperature of 37 ° C, then you need to read our article, in which we will try to reveal the rules of thermometry, and you will also learn what to do if the temperature is 37 degrees for three or more days.
Thermometry rules
A thermometer indicator of 37 in a child is a fairly common phenomenon, especially at the age of several months. The reason for this is that the child has not improved thermoregulation. This is normal and you should not panic about it. Also, “increased” indicators can be observed after physical overwork. For example, a child of 5 years old, he played active games in the yard for two hours in a row, ran, jumped, chased the ball, and suddenly got tired. Naturally, his cheeks turned red, he tries to lie down or sit down, becomes less active. What is the first thing mom does? Measures body temperature. Indicator 37 alarms her and this is quite natural. But, in this case, it is quite normal. Therefore, never take a child's temperature:
After active play
after crying and during it,
while taking a meal.
Important! Body temperature measurements can only be taken when the child is calm.
You need to take out a thermometer and put it into the child’s armpit only if the child’s behavior is alarming and the following symptoms are present:
Decreased appetite.
lethargy and drowsiness,
irritability,
tearfulness,
malaise.
Only after thermometry, if the child has an elevated temperature, can we say that the baby is sick and he needs to consult a doctor. Consider the main reasons that can cause subfebrile body temperature.
The main causes of fever
A temperature of 37 without symptoms in a child that could lead to the correct thought and determine the cause of this condition, in most cases, the first day is observed. Then, other signs should join the temperature to help determine the correct diagnosis. But self-medication, especially when it comes to children, is by no means impossible. At the same time, each of the parents should know the main reasons that can provoke a slight rise in the mercury column.
The main causes of subfebrile temperature
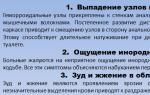
When it comes to crumbs of 6-9 months, a slight increase in the mercury column can be observed during teething. The baby becomes restless, pulls all the toys into her mouth, is naughty, cries. But the main symptom is increased salivation, swelling and redness of the gums. In this state, the temperature can rise in the range of 37.2 - 38.5 ° C.
In addition, the following pathologies can become the causes of hyperthermia:
Allergy,
infection,
tumor process,
acute form of inflammatory disease,
chronic form of the disease at the stage of exacerbation,
surgical pathology,
endocrine disorder,
immunodeficiency.
The most common illness among children is the common cold, especially when the weather is bad. This disease is transmitted by airborne droplets and is accompanied by other symptoms such as cough, runny nose, general malaise and headaches.
Similar symptoms can be observed in childhood infectious diseases. But, most often, such a disease begins with an elevated temperature, which lasts for several days (2-3 days), and only after that characteristic rashes can be noticed on the child's body. Children at any age suffer from childhood infectious diseases, and body temperature can range from 37.2 to 39 degrees, depending on the severity of the course, comorbidities and age. A child at 3 years of age is much easier to tolerate infectious diseases than a teenager at 9-12 years old. Therefore, treatment should only be carried out by a doctor, especially if the temperature does not rise above 37.2 degrees for several days.
A characteristic sign of childhood infectious diseases is a sharp malaise and a deterioration in general well-being. In some cases, the temperature may not even rise or rise slightly. Therefore, a doctor's call is simply necessary. Only with its help it is possible to accurately establish the true cause of the ailment by the external signs of the rash, carry out the necessary diagnostics and prescribe the correct treatment.
But, the presence of symptoms of intoxication requires that the baby be provided with abundant nutrition, due to which the process of removing bacteria and viruses from the body will be accelerated.
temperature tail
Sometimes parents ask why, after a sore throat, the temperature can exceed the norm by 3-5 divisions and is 36.9-37.2 ° C. This condition is observed quite often and, according to doctors, this is the norm. This indicator indicates that the child has reduced immunity. In the event that there are no additional symptoms, the "temperature tail" can persist from several days to 2-3 months, after which it will return to normal. At the same time, parents should do everything to strengthen the immune system: review the child's diet, develop a balanced diet, etc.
Complication
In the case when, after the illness, the temperature rises again after two days, then a cough joins it on the 4-5th day, then most likely the doctors will suspect complications of the disease in the form of pneumonia or bronchitis. After a professional diagnosis, the child will be prescribed additional treatment.
Temperature 37 keeps for a very long time
Separately, let's talk about such a symptom as a slightly high temperature, which can last for a long time (9-10 months), and sometimes more than a year.
If the thermometer stays above the norm for 4 months, then this symptom may indicate the development of the following pathologies:
viral hepatitis,
oncology,
tuberculosis,
autoimmune disease,
systemic lupus erythematosus,
pathology of kidney function,
increased thyroid function.
In order not to miss the development of one of the above diseases, the child should be brought to the pediatrician for examination at the first symptoms of malaise.
1. Slight icterus of the sclera and a temperature of 37 ° C in children under 1 year of age require a full range of examinations for autoimmune disease or viral hepatitis.
2. Sleep disturbance, irritability, small rash on the body - helminths or allergies.
3. Coughing, slight malaise and sweating in children under 4 months of age require additional examination of the lungs.
Therefore, regardless of the age of the child (4 months or 9 years), with a slight increase in temperature, which occurs without symptoms and lasts for the second or fifth month, consult a doctor. In any case, the child's behavior will be changed, he will become more passive, irritable and sleepy. Everything should be paid attention to and timely conduct thermometry.
The examination includes:
laboratory tests (blood, urine),
analysis of feces for the presence of worms,
fluorography,
electrocardiogram,
ultrasound.
In addition, the child must be shown:
neurologist,
infectious disease specialist
endocrinologist,
ENT.
What to do and how to treat the disease that caused the increase in body temperature, the doctor will decide after a full course of examination.
A high temperature in a child always causes excitement in the mother, especially if it lasts for several days or longer. However, a temperature of 37 in a child is not always an indicator of illness when it comes to a newborn baby and a baby. In a baby up to a year old, a constant temperature can range from 34.6 to 37.3 degrees without symptoms due to the imperfection of the thermoregulation system. Consider the question - why a child can have a temperature of 37 for a long time, and what to do to reduce it.
Temperature norm
First, find out what is the norm for children of different ages. Up to a year in children, a temperature of 37 does not indicate inflammation or a latent disease. During this period, babies may suddenly have a fever for various reasons:
- overwork;
- overheating or heat stroke;
- reaction to vaccinations;
- food/chemical allergies;
- teeth are being cut;
- massotherapy;
- other reasons.
In a month-old baby, the thermometer can show a mark of 38 degrees, and during the day the temperature can change many times. Until the process of thermoregulation improves, the jumps will continue - both at 6 and at 8 months.
In older children (after 1.5 - 2 years), the mark 37 on the thermometer indicates a sluggish process of inflammation, especially if the temperature lasts a week or more. Scientifically, this temperature is called subfebrile. The reasons may be different, therefore, to determine the state of health, it is necessary to consult a pediatrician.
Doctors give the following classification of body temperatures:
- low - from 35.5 and below;
- normal - 35.6 to 37;
- subfebrile - from 37 to 37.9;
- febrile - from 38 and above.
Sometimes doctors talk about subfebrile condition only relative to the mark of 37.5. Contrary to popular belief, not 36.6, but a temperature of 37 degrees is considered normal. This indicator is typical for most cases. The thermometer can rise and fall during the day by 0.5 degrees or by one. The lowest rate is in the morning, by the evening the norm may deviate by a whole degree.
What is subfebrile condition
We can talk about this phenomenon if the child has a temperature of 37 for 2 weeks, up to a month or longer. However, this applies to children in whom the mark on the thermometer is 36.6. It is worth noting that without a reason, fever or fever does not rise. Mom should consult a pediatrician about the condition of the child.
What is the best way to take a child's temperature? A mercury thermometer is placed in the armpit, in the rectal passage it is necessary to measure with an electronic thermometer. However, the readings of the thermometer in different parts of the body will be different - you should be aware of this. For example, with a rectal measurement, the reading will be a degree higher than in the armpit.
Important! After the crying and screaming of the child, the thermometer readings will be inaccurate - 0.5 or 1 degree higher. Electronic thermometers often give readings with a large error.
You can also measure the temperature in the mouth (using an electronic thermometer), but the reading will differ by 0.5 degrees in contrast to the readings in the armpit. Study this question in detail before you panic.
The causes of subfebrile condition can be different:
- infectious;
- non-infectious;
- autoimmune (rare);
- medication.
Important! If the temperature of 37 is not accompanied by pain and malaise, there is no reason to worry.
When should you worry? Subfebrile condition may be the result of some pathologies:
- ENT diseases;
- carious lesions of the teeth;
- pathology of the gastrointestinal tract;
- diseases of the urinary system;
- the appearance of abscesses after injections.
Subfebrile condition without accompanying symptoms of malaise is considered harmless and cannot be treated. The temperature remaining at around 37 may be a manifestation of the characteristics of the child's body. However, one should not rely on the features of the development of the body - you need to show the baby to the pediatrician and undergo a laboratory examination.
Symptoms of the disease
A completely different picture emerges at a temperature of 37 and a painful condition. This may indicate the following pathologies:
In a child, a temperature of 37.2 can last 1 and 4 months after taking antibiotics. This is not considered a pathology and goes away by itself, it can also go away in the third month after the treatment of a viral disease. Doctors call this condition "temperature tail".
If a child has a temperature of 37.5 after completion of treatment, we can talk about a relapse of the disease - re-infection or the onset of a complication.
Children in whom the temperature has given a complication in the form of convulsions need to bring down the fever at around 37.5. There is intolerance to hyperthermia, to which the body reacts very hard - in these cases, antipyretics are simply necessary at the first manifestations of fever.
How to get rid of the temperature
Is it necessary to give an antipyretic when the mark on the thermometer is 37.5 - 37.8? If your child is developing normally, it is not recommended to bring down a slight increase in temperature. This is due to the activity of the immune system and the production of interferon: you can not knock down natural processes. By giving medicine, you are doing a disservice to the immune system.
Note! Babies up to three months old are given antipyretics at 38 and above, all other children are knocked down at 39 degrees.
Instead of antipyretic drugs for subfebrile condition, you need to provide the child with maximum comfort:
- humidify the room;
- remove excess clothing (do not wrap);
- give compote or juice (you can not give raspberries);
- provide peace.
Remember that young children do not have developed or poorly developed sweat glands, so they have nothing to sweat with. In this case, raspberry decoction will not help. An older child can be given raspberries, before drinking enough water - so that there is something to sweat.
With hyperthermia, it is forbidden to give raspberries. First, it increases perspiration. Secondly, internal heat dries up fluid in the body. If you give your child raspberries to drink, there is a risk of dehydration. At a low temperature at the beginning of a cold, raspberries can be given. But if the hyperthermia has been going on for a week or two, raspberries won't help.
What medicines can children take? Doctors allow only two types of antipyretics - based on paracetamol and based on ibuprofen. Other remedies for hyperthermia should not be given to children: they cause dangerous complications and side effects.
We found out that a low temperature is kept in children for a variety of reasons. It can appear on the first or second day after vaccination, with mild SARS and with a latent form of internal inflammatory processes. In infants up to two years old, the processes of thermoregulation are not balanced, therefore, a slightly elevated temperature does not indicate a disease, but an imperfection of the body. Always be guided by the child's well-being: the first criterion is that he should be cheerful, 2 that there are no symptoms of diseases.
If a low temperature persists for 3 days after vaccination or after healing from a cold, there is nothing to worry about in this condition. And if subfebrile condition is already kept for 5 days, for example, the temperature is 37.7 in a child? In order not to worry, contact your pediatrician. If the baby feels comfortable, don't worry. If he shows obvious signs of illness, give an antipyretic and call an ambulance.
Of particular danger is a prolonged subfebrile condition in an adult child. This may be a symptom of a serious pathology of the internal organs. If a low temperature persisted for a month after taking antibiotics, there is no danger in this - the child's immunity simply decreased. The next reason for this state is the “temperature tail”. But if the fifth week has already gone after recovery, and subfebrile condition is holding on, it means that not everything is in order with the child - take him for an examination.
Temperature increase body to low subfebrile numbers - a fairly common phenomenon. It can be associated both with various diseases, and be a variant of the norm, or be an error in the measurements.
In any case, if the temperature is kept at 37oC, it is necessary to report this to a qualified specialist. Only he, after conducting the necessary examination, can say whether this is a variant of the norm, or indicates the presence of a disease.
Temperature: what can it be?
It should be borne in mind that body temperature is a variable value. Fluctuations during the day in different directions are acceptable, which is quite normal. None
symptoms it is not followed. But a person who first discovered a constant temperature of 37
C, may be extremely concerned about this.
A person's body temperature may be as follows:1. Reduced (less than 35.5oC).
2. Normal (35.5-37
3. Increased:
- subfebrile (37.1-38oC);
- febrile (above 38oC).
Often, the results of thermometry in the range of 37-37.5 ° C are not even considered pathology by specialists, calling only data of 37.5-38 ° C as subfebrile temperature.
What you need to know about normal temperature:
- According to statistics, the most common normal body temperature is 37oC, not 36.6oC, contrary to popular belief.
- The norm is physiological fluctuations in thermometry during the day in the same person within 0.5 ° C, or even more.
- Lower readings are usually observed in the morning hours, while the body temperature in the afternoon or evening can be 37oC or slightly higher.
- In deep sleep, thermometry readings may be 36oC or less (as a rule, the lowest readings are noted between 4 and 6 o'clock in the morning, but 37oC and above in the morning can indicate pathology).
- The highest measurements are often recorded from about 4 pm until night (for example, a constant temperature of 37.5oC in the evening may be normal).
- In old age, the normal body temperature may be lower, and its daily fluctuations are not so pronounced.
Whether an increase in temperature is a pathology depends on many factors. So, a long-term temperature of 37oC in a child in the evening is a variant of the norm, and the same indicators in an elderly person in the morning most likely indicate a pathology.
Where can you measure body temperature:
In the armpit. Although this is the most popular and simple measurement method, it is the least informative. The results can be affected by humidity, room temperature and many other factors. Sometimes there is a reflex increase in temperature during the measurement. This may be due to excitement, for example, from a visit to the doctor. With thermometry in the oral cavity or rectum, there can be no such errors.
In the mouth (oral temperature): its performance is usually 0.5
C higher than defined in the armpit.
In the rectum (rectal temperature): Normal is 0.5
C is higher than in the mouth and, accordingly, by 1
C higher than in the armpit.
It is also quite reliable to determine the temperature in the ear canal. However, for an accurate measurement, a special thermometer is required, so this method is practically not used at home.
It is not recommended to take measurements of oral or rectal temperature with a mercury thermometer - an electronic device should be used for this. For thermometry in infants, there are also electronic dummy thermometers.
Do not forget that the body temperature of 37.1-37.5 ° C may be associated with an error in the measurement, or talk about the presence of pathology, for example, about an infectious process in the body. Therefore, expert advice is still required.
Is 37oC temperature normal?
If the thermometer is 37-37.5
C - do not get upset and panic. Temperature over 37
C can be related to measurement errors. In order for thermometry to be accurate, the following rules must be observed:
1. The measurement should be carried out in a calm, relaxed state, not earlier than 30 minutes after physical activity (for example, after an active game, a child’s temperature can be 37-37.5
C and above).
2. In children, measurement data can be significantly increased after screaming and crying.
3. It is better to carry out thermometry at about the same time, since low rates are more often noted in the morning, and by the evening the temperature usually rises to 37
4. When taking thermometry in the armpit, it must be completely dry.
5. In cases where the measurement is taken in the mouth (oral temperature), it should not be taken after eating or drinking (especially hot), if the patient is short of breath or breathes through the mouth, and also after smoking.
6. Rectal temperature may rise by 1-2
C or more after exercise, hot bath.
7. Temperature 37
C or slightly higher can be after eating, after physical activity, against the background of stress, excitement or fatigue, after exposure to the sun, while in a warm, stuffy room with high humidity or, conversely, excessively dry air.
Another common reason for a temperature of 37oC and above can be a faulty thermometer. This is especially true for electronic devices, which quite often give an error in the measurement. Therefore, when receiving high readings, determine the temperature of another family member - suddenly it will also be too high. And it is even better that in this case there is always a working mercury thermometer in the house. When an electronic thermometer is still indispensable (for example, to determine the temperature of a small child), immediately after purchasing the device, take measurements with a mercury thermometer and an electronic one (you can use any healthy family member). This will make it possible to compare the results and determine the error in thermometry. When conducting such a test, it is better to use thermometers of different designs; you should not take the same mercury or electric thermometers.
A slight subfebrile temperature may be a variant of the norm in the following cases:
- A temperature of 37oC in an adult may be associated with stress, exercise, or chronic fatigue.
- In women, thermometry indicators fluctuate in accordance with the phases of the menstrual cycle. So, they are highest in the second phase (after ovulation), approximately between the 17th and 25th day of the cycle. They are accompanied by relevant basal temperature data, such as 37.3°C and above.
- Women during menopause often have a temperature of 37°C or more, which accompanies other symptoms of this condition, such as "hot flashes" and sweating.
- A temperature of 37-37.5 ° C in a one-month-old child is often a variant of the norm for him, and indicates the immaturity of thermoregulation processes. This is especially true for premature babies.
- The temperature of 37.2-37.5 ° C in a pregnant woman is also a variant of the norm. Usually, such indicators are recorded in the early stages, but they can persist until the very birth.
- A body temperature of 37oC in a breastfeeding woman is also not a pathology. Especially it can rise in the days of "milk flushes". However, if chest pain appears against this background, and the temperature rises above 37 ° C (often to febrile figures), this may be a sign of purulent mastitis, and requires urgent medical attention.
All these conditions are not dangerous for humans, and are associated with the course of natural physiological processes. However, whether the body temperature is 37.0 ° C or slightly above the normal variant, only a doctor can determine.
Pathological causes
Often the temperature is 37-37.5
Subfebrile fever in infectious diseases:
1.
Respiratory infections. The most common of these are common
With a mild course of the disease, there may be a temperature of 37
C or slightly higher, accompanied by
runny nose
Enlarged lymph nodes, aching muscles and lower back, as well as other manifestations of infection. Subfebrile fever may also accompany chronic bronchitis,
sinusitis
In some cases, when
pneumonia
keeps temperature 37
C. This usually indicates an atypical pathogen (for example,
chlamydia
or mycoplasma). Temperature 37-37.5
C may last several months, or even years, with a chronic infection such as
tuberculosis
Often it is asymptomatic, and is detected only due to subfebrile condition.
Urinary tract and kidney infections. With this pathology, a small subfebrile fever is often noted. This is especially true for inflammation.
Bladder
Temperature 37
C or higher often occurs when
It accompanies other characteristic symptoms of this condition. With inflammation
(pyelonephritis) fever usually reaches higher numbers, but with an exacerbation of a chronic process, it can also be subfebrile.
Infectious diseases of the gastrointestinal tract. When body temperature rises above 37
I have a stomachache
This can be a sign of a variety of diseases. So,
peptic ulcer
in the active stage may be accompanied by a slight subfebrile condition. Temperature 37-37.5
C, accompanied
diarrhea nausea
May be a manifestation
intestinal infections hepatitis
Diseases of the reproductive system. When women have 37-37.5
C temperature and
pain in lower abdomen
- this may be a sign of infectious diseases of the genital organs, for example,
vulvovaginitis
Temperature 37
C and above can be observed after procedures such as
Scraping. In men, fever may indicate
prostatitis
Diseases of the cardiovascular system. Infectious inflammatory processes in
heart muscle
often accompanied by low numbers of fever. But despite this, they are usually accompanied by such severe symptoms as
Heart rhythm disturbances
and a number of others.
Foci of chronic infection. They can be found in many organs. For example, if the body temperature is kept within 37.2
C, this may indicate the presence of a chronic
tonsillitisadnexitis
Prostatitis and other pathologies. After sanitation of the infectious focus, fever often disappears without a trace.
Children's infections. Often occurrence
and temperature 37
C or higher, may be a symptom
chickenpoxrubella
The rash usually appears at the height of the fever and may be accompanied by
and unpleasant sensations. However, the rash can be a symptom of more serious diseases (blood pathology,
sepsismeningitis
), so if it occurs, do not forget to call a doctor.
Often there are situations when, after an infectious disease, the temperature is 37oC and above for a long time. This feature is often referred to as the "temperature tail". Elevated temperature readings can persist for several weeks or months. Even after taking antibiotics against an infectious agent, 37oC may remain for a long time. This condition does not require treatment, and goes away on its own without a trace. However, if, along with low-grade fever, cough, rhinitis, or other symptoms of the disease are observed, this may indicate a relapse of the disease, the occurrence of complications, or indicate a new infection. It is important not to miss this condition, as it requires a visit to the doctor.
Other causes of subfebrile temperature in a child are often:
- overheat;
- reaction to prophylactic vaccination;
- teething.
Teething is one of the frequent causes of a child's temperature rise above 37-37.5oC. At the same time, thermometry data rarely reach numbers above 38.5 ° C, therefore, it is usually enough just to monitor the condition of the baby and use physical cooling methods. Temperatures above 37oC may occur after vaccination. Usually, the indicators are kept within subfebrile numbers, and with their further increase, you can give the child an antipyretic once. An increase in temperature as a result of overheating can be observed in those children who are excessively wrapped and dressed. It can be very dangerous and cause heat stroke. Therefore, when the baby overheats, it should be undressed first.
An increase in temperature can be observed in many non-communicable inflammatory diseases. As a rule, it is accompanied by other, rather characteristic signs of pathology. For example, a temperature of 37°C and blood-streaked diarrhea may be symptoms of ulcerative colitis or Crohn's disease. In some diseases, such as systemic lupus erythematosus, low-grade fever may appear several months before the first signs of the disease.
An increase in body temperature to low numbers is often noted against the background of allergic pathology: atopic dermatitis, urticaria and other conditions. For example, shortness of breath with difficulty exhaling, and a temperature of 37°C and above, can be observed with an exacerbation of bronchial asthma.
Subfebrile fever can be observed in the pathology of the following organ systems:
1. The cardiovascular system:
- VSD (vegetative dystonia syndrome) - a temperature of 37 ° C and a little higher may indicate sympathicotonia, and is often combined with high blood pressure, headaches and other manifestations;
- high blood pressure and temperature of 37-37.5 o C can be with hypertension, especially during crises.
Gastrointestinal tract: temperature 37
C or higher, and abdominal pain, may be signs of pathologies such as
pancreatitis
Non-infectious hepatitis and gastritis,
esophagitis
and many others.
Respiratory system: temperature 37-37.5
C can accompany
chronic obstructive pulmonary disease
4. Nervous system:
- thermoneurosis (habitual hyperthermia) - often observed in young women, and is one of the manifestations of autonomic dystonia;
- tumors of the spinal cord and brain, traumatic injuries, hemorrhages and other pathologies.
Endocrine system: fever may be the first manifestation of an elevated thyroid function (
hyperthyroidism
), Addison's disease (insufficient function of the cortex
adrenal glands
Kidney pathology: temperature 37
C and above can be a sign
glomerulonephritis
Dysmetabolic nephropathies,
urolithiasis
Sex organs: subfebrile fever can be observed with
ovarian cysts uterine myoma
and other pathologies.
Blood and immune system:
- a temperature of 37oC accompanies many immunodeficiency states, including oncology;
- a small subfebrile fever can occur with blood pathology, including with ordinary iron deficiency anemia.
Another condition in which body temperature is constantly kept at 37-37.5 ° C is oncological pathology. In addition to subfebrile fever, there may also be weight loss, loss of appetite, weakness, pathological symptoms from various organs (their nature depends on the location of the tumor).
Indicators of 37-37.5 ° C are a variant of the norm after a surgical operation. Their duration depends on the individual characteristics of the organism and the volume of surgical intervention. A slight fever may also be observed after some diagnostic manipulations, such as laparoscopy.
Which doctor should I contact with elevated body temperature?
Since an increase in body temperature can be due to a wide range of different causes, the choice of a specialist who needs to be contacted with a high temperature is determined by the nature of the person's other symptoms. Consider the doctors of which specialties you need to contact in various cases of fever:
- If, in addition to fever, a person has a runny nose, pain, sore or sore throat, cough, headaches, aching muscles, bones and joints, then it is necessary to contact general practitioner (make an appointment), since we are talking, most likely, about SARS, colds, flu, etc .;
- If an elevated body temperature is combined with a persistent cough, or a constant feeling of general weakness, or a feeling that it is difficult to inhale, or wheezing when breathing, then you should contact your general practitioner and phthisiatrician (sign up), since these signs can be symptoms of either chronic bronchitis, or pneumonia, or tuberculosis;
- If elevated body temperature is combined with pain in the ear, leakage of pus or fluid from the ear, runny nose, itching, soreness or sore throat, a feeling of mucus flowing along the back of the throat, a feeling of pressure, fullness or pain in the upper part of the cheeks (cheekbones under the eyes) or above the eyebrows, then you should refer to otolaryngologist (ENT) (make an appointment), since most likely we are talking about otitis media, sinusitis, pharyngitis or tonsillitis;
- If elevated body temperature is combined with pain, redness of the eyes, photophobia, leakage of pus or non-purulent fluid from the eye, you should contact ophthalmologist (make an appointment);
- If an elevated body temperature is combined with pain during urination, back pain, frequent urge to urinate, then you should consult a urologist / nephrologist (make an appointment) And venereologist (make an appointment), because a similar combination of symptoms may indicate either kidney disease or a sexual infection;
- If elevated body temperature is combined with diarrhea, vomiting, abdominal pain and nausea, then you should contact infectious disease doctor (make an appointment), since a similar set of symptoms may indicate an intestinal infection or hepatitis;
- If elevated body temperature is combined with moderate pain in the abdomen, as well as various dyspepsia phenomena (belching, heartburn, feeling of heaviness after eating, bloating, flatulence, diarrhea, constipation, etc.), then you should contact Gastroenterologist (make an appointment)(if there is none, then to the therapist), because. this indicates diseases of the digestive tract (gastritis, gastric ulcer, pancreatitis, Crohn's disease, etc.);
- If an elevated body temperature is combined with severe, unbearable pain in any part of the abdomen, then you should urgently contact surgeon (make an appointment), as this indicates a serious condition (for example, acute appendicitis, peritonitis, pancreatic necrosis, etc.) requiring immediate medical attention;
- If an elevated body temperature in women is combined with moderate or mild pain in the lower abdomen, discomfort in the genital area, unusual vaginal discharge, then you should contact gynecologist (make an appointment);
- If an elevated body temperature in women is combined with severe pain in the lower abdomen, bleeding from the genital organs, severe general weakness, then you should urgently contact a gynecologist, as these symptoms indicate a serious condition (for example, ectopic pregnancy, uterine bleeding, sepsis, endometritis after abortion, etc.), requiring immediate treatment;
- If an elevated body temperature in men is combined with pain in the perineum and in the prostate gland, then you should contact a urologist, as this may indicate prostatitis or other diseases of the male genital area;
- If elevated body temperature is combined with shortness of breath, arrhythmia, edema, then you should contact your therapist or cardiologist (make an appointment), as this may indicate inflammatory diseases of the heart (pericarditis, endocarditis, etc.);
- If elevated body temperature is combined with pain in the joints, rashes on the skin, marble coloration of the skin, impaired blood flow and sensitivity of the extremities (cold hands and feet, blue fingers, numbness, goosebumps, etc.), red blood cells or blood in the urine, pain when urinating, or pain in other parts of the body, you should contact rheumatologist (make an appointment), as this may indicate the presence of autoimmune or other rheumatic diseases;
- Temperature in combination with rashes or inflammations on the skin and ARVI phenomena may indicate various infectious or skin diseases (for example, erysipelas, scarlet fever, chickenpox, etc.), therefore, if such a combination of symptoms appears, you should contact a therapist, an infectious disease specialist and dermatologist (make an appointment);
- If elevated body temperature is combined with headaches, jumps in blood pressure, a feeling of interruptions in the work of the heart, then you should consult a therapist, as this may indicate vegetative-vascular dystonia;
- If elevated body temperature is combined with tachycardia, sweating, enlarged goiter, then you need to contact endocrinologist (make an appointment), as this may be a sign of hyperthyroidism or Addison's disease;
- If elevated body temperature is combined with neurological symptoms (for example, obsessive movements, coordination disorder, sensory impairment, etc.) or loss of appetite, unreasonable weight loss, then you should contact oncologist (make an appointment), as this may indicate the presence of tumors or metastases in various organs;
- An elevated temperature, combined with very poor health, which worsens over time, is a reason to immediately call an ambulance, regardless of what other symptoms a person has.
What tests and diagnostic procedures can be prescribed by doctors when the body temperature rises to 37-37.5oC?
Since body temperature can rise against the background of a wide range of various diseases, the list of studies that a doctor prescribes to identify the causes of this symptom is also very wide and variable. However, in practice, doctors do not prescribe the entire list of examinations and tests that can theoretically help identify the cause of elevated body temperature, but use only a limited set of certain diagnostic tests that most likely allow you to identify the source of temperature. Accordingly, for each specific case, doctors prescribe a different list of tests, which are selected in accordance with the accompanying symptoms that a person has in addition to fever, and indicating the affected organ or system.
Since the most common elevated body temperature is due to inflammatory processes in various organs, which can be either infectious (for example, tonsillitis, rotavirus infection, etc.) or non-infectious (for example, gastritis, ulcerative colitis, Crohn's disease, etc.) .), then always if it is present, regardless of the accompanying symptoms, a general blood test and a general urinalysis are prescribed, allowing you to find out in which direction the further diagnostic search should go and what other tests and examinations are necessary in each specific case. That is, in order not to prescribe a large number of studies of various organs, they first do a general analysis of blood and urine, which allow the doctor to understand in which direction to “look for” the cause of elevated body temperature. And only after identifying an approximate spectrum of possible causes of temperature, other studies are prescribed to clarify the pathology that caused hyperthermia.
The indicators of a general blood test make it possible to understand whether the temperature is caused by an inflammatory process of an infectious or non-infectious origin, or is not associated with inflammation at all.
So, if the ESR is increased, then the temperature is due to the inflammatory process of an infectious or non-infectious origin. If the ESR is within the normal range, then the elevated body temperature is not associated with the inflammatory process, but is due to tumors, vegetative-vascular dystonia, endocrine diseases, etc.
If, in addition to the accelerated ESR, all other indicators of the general blood test are within the normal range, then the temperature is due to a non-infectious inflammatory process, for example, gastritis, duodenitis, colitis, etc.
If anemia is detected according to the general blood test, and other indicators, except for hemoglobin, are normal, then the diagnostic search is completed, since the fever is caused precisely by the anemic syndrome. In such a situation, anemia is treated.
A general urine test allows you to understand whether there is a pathology of the organs of the urinary system. If there is such an analysis, then other studies are carried out in the future to clarify the nature of the pathology and begin treatment. If the urine tests are normal, then to find out the cause of the elevated body temperature, they do not conduct a study of the organs of the urinary system. That is, a general urinalysis will immediately identify the system in which the pathology caused an increase in body temperature, or, on the contrary, dismiss suspicions about diseases of the urinary tract.
Having determined fundamental points from a general analysis of blood and urine, such as infectious or non-infectious inflammation in humans, or a non-inflammatory process at all, and whether there is a pathology of the urinary organs, the doctor prescribes a number of other studies to understand which organ is affected. Moreover, this list of examinations is already determined by the accompanying symptoms.
Below we give options for the lists of tests that a doctor can prescribe at elevated body temperature, depending on other concomitant symptoms that a person has:
- With a runny nose, sore throat, sore or sore throat, cough, headache, aching muscles and joints, only a general blood and urine test is usually prescribed, since such symptoms are caused by SARS, influenza, colds, etc. However, during an influenza epidemic, a blood test may be ordered to detect the influenza virus to determine whether a person is dangerous to others as a source of influenza. If a person often suffers from colds, then he is prescribed immunogram (to sign up)(total lymphocyte count, T-lymphocytes, T-helpers, T-cytotoxic lymphocyte, B-lymphocytes, NK cells, T-NK cells, HCT test, phagocytosis assessment, CEC, immunoglobulins of IgG, IgM, IgE, IgA classes ) to determine which parts of the immune system are not working properly and, accordingly, which immunostimulants need to be taken to normalize the immune status and stop frequent episodes of colds.
- At a temperature combined with a cough or a constant feeling of general weakness, or a feeling that it is difficult to inhale, or wheezing when breathing, it is imperative to do chest x-ray (book) and auscultation (listen with a stethoscope) of the lungs and bronchi to find out if the person has bronchitis, tracheitis, pneumonia, or tuberculosis. In addition to X-ray and auscultation, if they did not give an accurate answer or their result is doubtful, the doctor may prescribe sputum microscopy, the determination of antibodies to Chlamydophila pneumoniae and respiratory syncytial virus in the blood (IgA, IgG), the presence of mycobacterium DNA to distinguish between bronchitis, pneumonia and tuberculosis and Chlamydophila pneumoniae in sputum, bronchial swabs, or blood. Tests for the presence of mycobacteria in sputum, blood, and bronchial washings, as well as sputum microscopy, are usually prescribed for suspected tuberculosis (either asymptomatic persistent fever or fever with cough). But tests for the determination of antibodies to Chlamydophila pneumoniae and respiratory syncytial virus in the blood (IgA, IgG), as well as the determination of the presence of Chlamydophila pneumoniae DNA in sputum, are carried out to diagnose bronchitis, tracheitis and pneumonia, especially if they are frequent, long-lasting or not treatable antibiotics.
- Temperature, combined with a runny nose, a feeling of mucus running down the back of the throat, a feeling of pressure, fullness or pain in the upper part of the cheeks (cheekbones under the eyes) or above the eyebrows, requires a mandatory x-ray of the sinuses (maxillary sinuses, etc.) (make an appointment) to confirm sinusitis, frontal sinusitis or another type of sinusitis. With frequent, long-term or antibiotic-resistant sinusitis, the doctor may additionally prescribe the determination of antibodies to Chlamydophila pneumoniae in the blood (IgG, IgA, IgM). If the symptoms of sinusitis and fever are combined with blood in the urine and frequent pneumonia, then the doctor may prescribe a blood test for antineutrophil cytoplasmic antibodies (ANCA, pANCA and cANCA, IgG), since systemic vasculitis is suspected in such a situation.
- If an elevated temperature is combined with a feeling of mucus running down the back of the throat, a feeling that cats are scratching in the throat, sore and tickle, then the doctor prescribes an ENT examination, takes a smear from the oropharyngeal mucosa for bacteriological culture in order to determine the pathogenic microbes that caused inflammatory process. An examination is usually carried out without fail, but a smear from the oropharynx is not always taken, but only if a person complains of the frequent occurrence of such symptoms. In addition, with the frequent occurrence of such symptoms, their persistent failure even with antibiotic treatment, the doctor may prescribe the determination of antibodies to Chlamydophila pneumonia and Chlamydia trachomatis (IgG, IgM, IgA) in the blood, tk. these microorganisms can provoke chronic, often recurrent infectious and inflammatory diseases of the respiratory system (pharyngitis, otitis media, sinusitis, bronchitis, tracheitis, pneumonia, bronchiolitis).
- If an elevated temperature is combined with pain, sore throat, enlarged tonsils, the presence of plaque or white plugs in the tonsils, a constantly red throat, then an ENT examination is mandatory. If such symptoms are present for a long time or often appear, then the doctor prescribes a smear from the oropharyngeal mucosa for bacteriological culture, as a result of which it will become known which microorganism provokes the inflammatory process in the ENT organs. If the sore throat is purulent, then the doctor must prescribe blood for the ASL-O titer in order to identify the risk of developing complications of this infection, such as rheumatism, glomerulonephritis, and myocarditis.
- If the temperature is combined with pain in the ear, outflow of pus or any other liquid from the ear, then the doctor must conduct an ENT examination. In addition to the examination, the doctor most often prescribes a bacteriological culture of discharge from the ear to determine which pathogen caused the inflammatory process. In addition, tests can be prescribed to determine antibodies to Chlamydophila pneumonia in the blood (IgG, IgM, IgA), for the ASL-O titer in the blood, and for the detection of type 6 herpes virus in saliva, scrapings from the oropharynx and blood. Tests for antibodies to Chlamydophila pneumonia and for the presence of the herpes virus type 6 are performed to identify the microbe that caused otitis media. However, these tests are usually prescribed only for frequent or long-term otitis media. A blood test for ASL-O titer is prescribed only for purulent otitis media to identify the risk of developing complications of streptococcal infection, such as myocarditis, glomerulonephritis and rheumatism.
- If the elevated body temperature is combined with pain, redness in the eye, as well as the discharge of pus or other liquid from the eye, then the doctor performs a mandatory examination. Next, the doctor may prescribe a culture of the detachable eye for bacteria, as well as a blood test for antibodies to adenovirus and for the content of IgE (with particles of dog epithelium) in order to determine the presence of adenovirus infection or allergies.
- When elevated body temperature is combined with pain during urination, back pain or frequent trips to the toilet, the doctor will first of all and without fail prescribe a general urinalysis, determination of the total concentration of protein and albumin in daily urine, urinalysis according to Nechiporenko (sign up), Zimnitsky's test (sign up), as well as a biochemical blood test (urea, creatinine). These tests in most cases allow you to determine the existing disease of the kidneys or urinary tract. However, if the listed tests did not clarify, then the doctor may prescribe bladder cystoscopy (make an appointment), bacteriological culture of urine or scrapings from the urethra to identify a pathogenic agent, as well as the determination by PCR or ELISA of microbes in scrapings from the urethra.
- If you have a fever that is accompanied by pain when urinating or frequent trips to the toilet, your doctor may order tests for various sexually transmitted infections (such as gonorrhea (sign up), syphilis (sign up), ureaplasmosis (sign up), mycoplasmosis (sign up), candidiasis, trichomoniasis, chlamydia (sign up), gardnerellosis, etc.), since such symptoms may also indicate inflammatory diseases of the genital tract. For tests for genital infections, the doctor may prescribe vaginal discharge, semen, prostate secretions, a urethral swab, and blood. In addition to analyzes, it is often prescribed Ultrasound of the pelvic organs (make an appointment), which allows you to identify the nature of the changes occurring under the influence of inflammation in the genital organs.
- At elevated body temperature, which is combined with diarrhea, vomiting, abdominal pain and nausea, the doctor first of all prescribes a stool test for scatology, a stool test for helminths, a stool test for rotavirus, a stool test for infections (dysentery, cholera, pathogenic strains of intestinal coli, salmonellosis, etc.), fecal analysis for dysbacteriosis, as well as scraping from the anus for sowing in order to identify the pathogen that provoked the symptoms of an intestinal infection. In addition to these tests, the infectious disease specialist prescribes blood test for antibodies to hepatitis A, B, C and D viruses (sign up), since such symptoms may indicate acute hepatitis. If a person, in addition to fever, diarrhea, abdominal pain, vomiting and nausea, also has yellowness of the skin and sclera of the eyes, then only blood tests for hepatitis (antibodies to hepatitis A, B, C and D viruses) are prescribed, as this indicates about hepatitis.
- In the presence of elevated body temperature, combined with abdominal pain, dyspepsia (belching, heartburn, flatulence, bloating, diarrhea or constipation, blood in the stool, etc.), the doctor usually prescribes instrumental studies and a biochemical blood test. With belching and heartburn, a blood test for Helicobacter pylori is usually prescribed and fibrogastroduodenoscopy (FGDS) (make an appointment), which allows you to diagnose gastritis, duodenitis, stomach or duodenal ulcer, GERD, etc. With flatulence, bloating, periodic diarrhea and constipation, the doctor usually prescribes a biochemical blood test (amylase, lipase, AST, ALT, alkaline phosphatase activity, protein, albumin, bilirubin concentration), urinalysis for amylase activity, fecal analysis for dysbacteriosis and coprology and Ultrasound of the abdominal organs (make an appointment), which allow diagnosing pancreatitis, hepatitis, irritable bowel syndrome, biliary dyskinesia, etc. In complex and incomprehensible cases or suspicion of tumor formations, the doctor may prescribe MRI (make an appointment) or x-ray of the digestive tract. If there is frequent bowel movement (3-12 times a day) with unformed feces, ribbon stools (feces in the form of thin ribbons) or pain in the rectal area, then the doctor prescribes colonoscopy (make an appointment) or sigmoidoscopy (make an appointment) and analysis of feces for calprotectin, which reveals Crohn's disease, ulcerative colitis, intestinal polyps, etc.
- At elevated temperature, in combination with moderate or mild pain in the lower abdomen, discomfort in the genital area, abnormal vaginal discharge, the doctor will definitely prescribe, first of all, a smear from the genital organs and ultrasound of the pelvic organs. These simple studies will allow the doctor to figure out what other tests are needed to clarify the existing pathology. In addition to ultrasound and smear for flora (make an appointment) the doctor may prescribe tests for sexual infections (sign up)(gonorrhea, syphilis, ureaplasmosis, mycoplasmosis, candidiasis, trichomoniasis, chlamydia, gardnerellosis, fecal bacteroids, etc.), for the detection of which they give vaginal discharge, scraping from the urethra or blood.
- At elevated temperature, combined with pain in the perineum and prostate in men, the doctor will prescribe a general urine test, prostate secret for microscopy (make an appointment), spermogram (sign up), as well as a smear from the urethra for various infections (chlamydia, trichomoniasis, mycoplasmosis, candidiasis, gonorrhea, ureaplasmosis, fecal bacteroids). In addition, the doctor may prescribe an ultrasound of the pelvic organs.
- At a temperature in combination with shortness of breath, arrhythmia and edema, it is imperative to do ECG (sign up), chest x-ray, Ultrasound of the heart (make an appointment), as well as take a general blood test, a blood test for C-reactive protein, rheumatic factor and titer ASL-O (sign up). These studies allow you to identify the existing pathological process in the heart. If the studies do not allow clarifying the diagnosis, then the doctor may additionally prescribe a blood test for antibodies to the heart muscle and antibodies to Borrelia.
- If fever is combined with skin rashes and symptoms of SARS or influenza, then the doctor usually prescribes only a general blood test and examines rashes or redness on the skin in various ways (under a magnifying glass, under a special lamp, etc.). If there is a red spot on the skin that grows over time and is painful, the doctor will prescribe an ASL-O titer test to confirm or refute erysipelas. If the rashes on the skin cannot be identified during the examination, then the doctor can take a scraping and prescribe its microscopy to determine the type of pathological changes and the causative agent of the inflammatory process.
- When temperature is combined with tachycardia, sweating and enlarged goiter, Ultrasound of the thyroid gland (make an appointment), as well as take a blood test for the concentration of thyroid hormones (T3, T4), antibodies to steroid-producing cells of the reproductive organs and cortisol.
- When the temperature is combined with headaches, jumps in blood pressure, a feeling of interruptions in the work of the heart, the doctor prescribes blood pressure control, ECG, ultrasound of the heart, ultrasound of the abdominal organs, REG, as well as a complete blood count, urine and biochemical blood test (protein, albumin , cholesterol, triglycerides, bilirubin, urea, creatinine, C-reactive protein, AST, ALT, alkaline phosphatase, amylase, lipase, etc.).
- When the temperature is combined with neurological symptoms (for example, coordination disorder, sensitivity deterioration, etc.), loss of appetite, unreasonable weight loss, the doctor will prescribe a general and biochemical blood test, a coagulogram, as well as an x-ray, Ultrasound of various organs (make an appointment) and, possibly, tomography, since such symptoms can be a sign of cancer.
- If the temperature is combined with pain in the joints, rashes on the skin, marble coloration of the skin, with impaired blood flow in the legs and arms (cold hands and feet, numbness and feeling of running "goosebumps", etc.), red blood cells or blood in the urine and pain in other parts of the body, then this is a sign of rheumatic and autoimmune diseases. In such cases, the doctor prescribes tests to determine whether a person has a joint disease or an autoimmune pathology. Since the spectrum of autoimmune and rheumatic diseases is very wide, the doctor first prescribes x-ray of joints (make an appointment) and the following non-specific tests: complete blood count, C-reactive protein, rheumatoid factor, lupus anticoagulant, antibodies to cardiolipin, antinuclear factor, IgG antibodies to double-stranded (native) DNA, ASL-O titer, antibodies to nuclear antigen, antineutrophil cytoplasmic antibodies (ANCA), antibodies to thyroperoxidase, the presence of cytomegalovirus, Epstein-Barr virus, herpes viruses in the blood. Then, if the results of the listed tests are positive (that is, markers of autoimmune diseases are found in the blood), the doctor, depending on which organs or systems have clinical symptoms, prescribes additional tests, as well as X-ray, ultrasound, ECG, MRI, to assess the degree of activity of the pathological process. Since there are many analyzes for detecting and evaluating the activity of autoimmune processes in various organs, we present them in a separate table below.
| Organ system | Analyzes to determine the autoimmune process in the organ system |
| Connective tissue diseases |
|
| Joint diseases |
|
| Antiphospholipid Syndrome |
|
| Vasculitis and kidney damage (glomerulonephritis, etc.) |
|
| Autoimmune diseases of the digestive tract |
|
| autoimmune liver disease |
|
| Nervous system |
|
| Endocrine system |
|
| Autoimmune skin diseases |
|
| Autoimmune diseases of the heart and lungs |
|
Temperature 37-37.5oС: what to do? How to bring down the temperature of 37-37.5oС? Reducing this temperature with drugs is not required. They are used only in cases of fever above 38.5oC. An exception is an increase in temperature in late pregnancy, in young children who have previously had febrile convulsions, as well as in the presence of severe diseases of the heart, lungs, and nervous system, which may worsen against a background of high fever. But even in these cases, it is recommended to reduce the temperature with medications only when it reaches 37.5 ° C and above.
The use of antipyretic drugs and other self-medication methods can make it difficult to diagnose the disease, as well as lead to unwanted side effects.
In all cases, the following guidelines must be followed:1. Think: Are you doing the right thermometry? The rules for taking measurements have already been mentioned above.
2. Try to change the thermometer to eliminate possible errors in the measurements.
3. Make sure that this temperature is not a variant of the norm. This is especially true for those who previously did not regularly measure the temperature, but revealed increased data for the first time. To do this, you need to contact a specialist to exclude the symptoms of various pathologies and prescribe an examination. For example, if the temperature is 37
C or slightly higher is constantly determined during pregnancy, while there are no symptoms of any diseases - most likely, this is the norm.
If the doctor has identified any pathology leading to an increase in temperature to subfebrile numbers, then the goal of therapy will be the treatment of the underlying disease. It is likely that after treatment, the temperature indicators will return to normal.
In what cases should you contact a specialist immediately:1. Subfebrile body temperature began to rise to febrile numbers.
2. Although the fever is mild, it is accompanied by other severe symptoms (severe cough, shortness of breath,
chest pain
Violation of urination, vomiting or diarrhea, signs of exacerbation of chronic diseases).
Thus, even a seemingly low temperature can be a sign of serious illness. Therefore, if you have any doubts about your condition, you should inform your doctor about them.
Prevention measures
Even if the doctor did not reveal any pathology in the body, and the constant temperature is 37-37.5
C is a variant of the norm, this does not mean that you can do nothing at all. Prolonged subfebrile indicators are chronic
stress
for the body.
To gradually bring the body back to normal, you should:
- timely identify and treat foci of infection, various diseases;
- avoid stress;
- to refuse from bad habits;
- observe the daily routine and get enough sleep;
- regularly engage in sports, hardening;
- spend more time outdoors.
All of these methods help to strengthen the immune system and train heat transfer processes. If these recommendations are followed, the body will return to normal.
ATTENTION! The information posted on our site is a reference or popular and is provided to a wide range of readers for discussion. The prescription of medicines should be carried out only by a qualified specialist, based on the history of the disease and the results of the diagnosis.
When a child's body temperature rises, then the parents at a subconscious level have an alarming state. This is normal, since even a slight deviation in a child's body temperature from normalized values is a precursor to the development of serious diseases. If the child has had a temperature of 37-37.5 degrees for 5 days, then you should inform the doctor about this or show him the baby. But in all cases, do you need to see a doctor, as well as the main causes of subfebrile hyperthermia in children, we will find out further.
What should be the temperature of the child
Body temperature is a variable value, which is especially important for a child's body. Throughout the day, its fluctuations are permissible, which is influenced by various factors:
- the child's condition;
- age;
- the temperature in the room or on the street where the child is;
- meal time.
There are the following temperature indicators in children:
- Reduced, while the thermometer will show a value below 36 degrees.
- Normal. These are values from 36 to 37, and for babies up to 37.4 degrees.
- Increased. It, in turn, is divided into subfebrile (37-38 degrees) and febrile (38 and above).
At the age of up to a year is normal, so if there are no signs of malaise, then parents have nothing to worry about. If the temperature is kept at 37 in a child older than 5 years, then here it is necessary to think about the fact that he develops a disease.
Before judging that a child has a temperature of 37 indicates a disease, it is necessary to take measurements correctly. What are the methods for measuring temperature in children, find out in more detail.
Where to measure the temperature of a child
The traditional method of measuring temperature in a child is to place the thermometer under the armpit. It is not difficult to measure a child older than 2-3 years in this way, but what about babies. Infants can also take temperature measurements under the arm, but the procedure must be carried out during the period when the baby is sleeping.
It is important to know! To obtain the most plausible thermometry information, it is necessary to take measurements during the child's sleep. The exception is the period of time when the baby is breastfeeding, and at the same time sleeping.
In addition to axillary temperature measurement, there are the following options:
- In the mouth. Oral temperature is usually 0.5-1 degree higher than axillary values.
- In the rectum. Rectal temperature is 1-1.2 degrees higher than axillary temperature. To measure it, you should use a special electronic thermometer.
- In the ear Children often measure the temperature in the ear, which allows you to get the most accurate information about thermometry. To take measurements, a special thermometer is required, which is inserted into the ear canal for a few seconds.

If, after the parents have measured the child's temperature, there are doubts, it is better to re-measure after a while. Very often, parents begin to panic, although they did not measure the temperature correctly.
It is important to know! To make sure the child is healthy or sick, you need to call a doctor or go to a hospital, where all assumptions will be dispelled.
Causes of subfebrile condition in children
Now let's look at all the possible reasons why a child has a temperature of 37-37.5 degrees for the fifth day. If for several days the child will keep hyperthermia at the level of 37-37.5 degrees, then you should not resort to the use of antipyretics.
It is important to know! You can only bring down febrile body temperature when the thermometer shows values of 38.5-39 degrees.
Measurement accuracy
The first reason that a child has 4 days of hyperthermia is an error or incorrect measurement. A family with children should have at least two thermometers. To make sure that the thermometer is functioning, use another one. Only after both thermometers show the same value, one can judge subfebrile condition. Most often, it is electronic thermometers that fail, so always keep a mercury device on hand.
You should also not forget about when measurements are taken. If the mother takes measurements of hyperthermia in the evening, then the readings will be elevated, because in the evening the body temperature rises. Measurements are best taken in the morning after 10 o'clock or in the afternoon, but not after eating. You can take measurements in two ways, which will increase the chances of obtaining reliable results.
It is important to know! If the parents are convinced that the baby really has subfebrile condition for more than 6 days, then it is necessary to notify the local doctor about this or go to the hospital.
Teething
The temperature that usually lasts for 4 days indicates that the baby's teeth are erupting. In this case, the age of the crumbs must comply with the following standards:
- from 3 months to 3 years, milk teeth climb in children, so parents should always be careful and learn to distinguish the appearance of the next tooth;
- from 6-7 years old, milk teeth begin to fall out, and molars appear in their place;
- the process of replacing milk teeth with molars lasts up to 10-15 years.
Almost 80% of all children endure the process of teething with the onset of fever, which is an absolutely normal physiological phenomenon. Another 10% of children endure the process of teething very difficult, so these children suffer from an increase in hyperthermia to febrile values. And only 10% of children tolerate the phenomenon of teething quite easily even without an increase in temperature.

It is not difficult to determine the signs of teething in children, for this it is enough to look into his oral cavity. If there are signs of redness and swelling of the gums, as well as excessive salivation, then the causes of low-grade fever are understandable. When teething, babies pull any objects into their mouths, which can lead to the penetration of pathogenic microbes into the body. The consequence of such unauthorized entry will be the development of an inflammatory process, which will lead to febrile hyperthermia.
It is important to know! When teething, it is possible to bring down the heat if the thermometer readings display a value above 38.5 degrees.
Overheating of the body
The fourth day the temperature can be kept due to overheating of the body. This is especially true if the temperature conditions where the baby is located are not observed. The optimal temperature in the room where the baby is located should correspond to the norm from 18 to 22 degrees. If the room is very hot, then subfebrile condition in a baby can be detected for a long time.
Often parents tend to dress their children warmly, hoping that in this way they are protected from the influence of negative factors. Children need to be dressed according to the weather, and if parents do not take this rule into account, then the consequence can be not only overheating, but also a cold against the background of excessive sweating. If the temperature kept for a long time at a subfebrile level, but when the child fell asleep, its value returned to normal, then there is no reason to panic. Prolonged exposure to the sun or in a hot room, active games, excessive wrapping of the child are all signs that the baby has an overheating of the body. To check whether the body of the crumbs is really overheated, you should remove warm clothes from it or transfer it to the shade. In this case, the thermometer readings will normalize within 1-2 hours, which will mean the presence of signs of overheating.
It is important to know! Overheating of the body is not as dangerous as heat or sunstroke, in the presence of which the baby may lose consciousness. Monitor the condition of your little one to prevent the development of serious complications.
Reaction to vaccination
The temperature cannot be kept for 4 days due to a reaction to the vaccine, so if parents have suspicions, it is better to consult a doctor. From the moment of birth, all children are subject to mandatory vaccination. Some vaccines are simple and harmless, but there are those that cause reactions in the body. Most often, such reactions manifest themselves in the form of subfebrile condition, which lasts no more than 2 days. This is a normal reaction of the body to the vaccine, so parents need not worry.
Another thing is when a baby has a fever for four days after vaccination. This can only mean that at the time of the introduction of the vaccine, the child picked up a virus or infection. Hyperthermia is a sign that the body is trying to fight pathogens. If hyperthermia lasts 6 days or more, then you need to inform the doctor. The body may need help in the form of antiviral or antibacterial drugs, but only as prescribed by a specialist.
Subfebrile condition in children due to various ailments
Allergic reactions can also be attributed to the above signs, but to determine them, you will need to carefully observe the baby. If symptoms of redness, swelling, fever, increased secretion of mucus from the nose and mouth are found, then the cause is most likely an allergic reaction. If all of the above signs are excluded, then the worst options should be considered - various diseases. Only a specialist can diagnose ailments, so parents should not try to make a diagnosis on their own, and even more so, prescribe treatment. Consider what kind of diseases provoke a temperature in children in the range of 37-37.5 degrees.
- Infectious diseases of the respiratory system. Most often, it manifests itself in the form of a disease such as SARS. With the development of this disease, after 1 laziness, symptoms of a runny nose and cough occur. If the acute form of ARVI becomes chronic, then the child may remain subfebrile not only for several days, but also for months. Usually, by subfebrile condition, they find out the presence of serious respiratory diseases, such as tuberculosis.
- Infectious ailments of the kidneys and urinary organs. With inflammation of the bladder in a child, the temperature may last for the sixth day or more. During the day, the temperature can decrease, and in the evening it can rise again to 37.5 degrees. Infectious diseases of the kidneys and urinary organs include diseases such as cystitis and pyelonephritis. It is in the presence of subfebrile condition that it is possible to determine these types of diseases.
- Infectious diseases of the gastrointestinal tract. If the child has a fever, and the stomach hurts, then it is necessary to look for the cause in the digestive system. Here, exacerbations of diseases such as gastritis, ulcers, poisoning, intestinal infections can occur. Infectious ailments of the gastrointestinal tract are manifested in the form of diarrhea and vomiting.
- Disorders of the cardiovascular system. This condition is especially relevant for children who were born with pathologies of the heart and vascular system. Children with congenital pathologies of the cardiovascular system require special attention and care.
- Children's infectious diseases. Subfebrile condition in children can be provoked against the background of exacerbation of infectious childhood diseases such as chickenpox, rubella, measles. Signs of these ailments is a rash all over the body, which occurs, most often, for 2-3 days.
In order to exclude the aforementioned ailments, you should visit a doctor. If the cause of the development of the disease is determined in a timely manner, then it will be much easier to eliminate it than when the disease goes into the acute stage.
In conclusion, it is important to note that despite the insignificance of a temperature of 37-37.5 degrees, one should promptly respond to its occurrence in a child. It is better to exclude serious pathologies immediately than to carry out long-term treatment later.