Joint mobility in divers at the stage of sports improvement. Methods for restoring a hand after a stroke
The musculoskeletal system is represented by a dynamic and static part that maintains the shape of the body. The axes of motion of the joints provide normal movement in space and vary from simple flexion to rotation. Mobility depends on the anatomical features, integrity and tone of adjacent muscles and ligaments.
What kinds exist?
Functional features, structure, localization and types of mobility are key factors in the formation of the classification. The division into types of joints takes place taking into account the following characteristics:
- the function being performed;
- structure;
- types of movements.
Classification based on functional characteristics distinguishes 3 types depending on the degree of their mobility. The fixed and inactive joints of the bones are located in the axial skeleton, provide its strength and protect the internal organs from injury. True or mobile are localized in the limbs and are characterized by a large amplitude (shoulder joint).
Based on the structural features, the following types of joints are distinguished:
 One of the types of joints is synovial.
One of the types of joints is synovial. - Fibrous. The simplest in structure. They imply the absence of a joint cavity and inactivity. Allocate syndesmosous, suture and rod fibrous.
- Cartilaginous. The bones are connected to each other with the help of hyaline cartilage.
- Synovial. Such an articulation of the bones is connected to form a synovial articular cavity filled with a special fluid. This substance provides smooth sliding of the bone surface. Among the synovial joints, flat, block-shaped hinge, condylar, saddle and ball joints are distinguished. The latter is able to move around its axis.
What provides mobility?
The main function of the musculoskeletal system is the ability to make movements in different directions. The process is controlled by the central nervous system, sending nerve impulses to adjacent muscles and ligaments. The ability to move and amplitude depend on the shape and type of the bone surface, the number of attached muscle fibers, their tone and attachment sites. The most mobile are the hinge joints.
What are the types of joint movements?
 The knee joint can flex and extend in the sagittal plane.
The knee joint can flex and extend in the sagittal plane. Anatomical features of different types of bone joints are reflected in their functionality. Types of movements in the joints are classified depending on the axis of their rotation. They are carried out only in the frontal, sagittal and vertical planes. The combined type of articulation of bones makes complex movements in the joints. Depending on the axis of rotation, the following types of mobility are distinguished:
Types of mobility restrictions and causes
The violation is called "contracture" and manifests itself in biomechanics, as a result of which the limb cannot perform a certain type of movement. Inactivity can be congenital or acquired. The cause of the acquired is trauma, dystrophic and inflammatory processes, paralysis, scars and wounds on the skin. Based on the inability to make movements along a certain axis, the following types of limited mobility are distinguished:
 The articulation may be limited in movement at the moment of extension.
The articulation may be limited in movement at the moment of extension. - Flexion. Inability to bend a limb.
- extensor. The joint does not fully flex.
- Leading and diverting. Difficult abduction of the limb to the side or inability to press against the body.
- Rotary. Complete immobility of the site.
Persistent restriction of movement in the joint without medical assistance leads to a number of complications. Inflammatory and dystrophic processes can spread to nearby tissues, and inactivity can flow into bone fusion. Possible complications can be prevented if assistance is provided when the first symptoms of contracture appear.
If you experience discomfort and stiffness in your back or limbs, you should immediately consult a doctor.
What to do with stiffness?
The limited mobility of the joints occurs due to a number of pathologies both in its cavity and in adjacent tissues. Treatment of contractures is aimed at eliminating the underlying cause and involves the use of pharmacological agents, physiotherapy and surgery. Physiological amplitude is restored by improving local blood circulation and innervation, removing interfering scars and adhesions. However, complications are possible when heat is applied to the elbow joint.
The question of age-related changes in the amplitudes of movements in large and small joints of the lower and upper extremities has not been sufficiently developed in the literature. One can only point to a number of works concerning age-related changes in the large joints of the limbs (Saario Zanri, 1961).
We carried out goniometric studies of the amplitudes of movements in large and small joints of the limbs in the population of Astrakhan (2800 people) aged from 1 to 84 years - 27 different amplitudes of movements in each age and sex group. In children under 6 years old, the amplitudes of passive movements in the joints were measured, starting from 7 years old - the maximum amplitudes of active movements.
The results of the variational-statistical analysis of the amplitudes of movements of the right limb joints are presented in tables 25-26. As in the analysis of mobility data for all parts of the spine, the above three phases of age-related changes in the amplitudes of movements in the joints can be distinguished here: 1) an increase phase, 2) a relative stabilization phase, and 3) a decrease phase. Heterochrony and different intensity of their change are also noted. In some amplitudes of movements, the phase of increase is short and lasts only up to 2-3 years of age, in others it is significant (up to 17-19 years). The phase of relatively stable condition can continue until the age of 30-59 years. In the elderly and senile age, there is already a significant decrease in mobility in the joints. Some ranges of motion have a high intensity of change, while others change relatively slightly. So, for example, the amplitude of extension in the wrist joint during the individual life of a person in males and females changes by 40.8 °, and the amplitude of flexion in this joint in men - by 23.3 °, in women - by 26.7 ° . The amplitude of extension in the metacarpophalangeal joints changes in males by 46.5°, in females - by 43.6°, while the amplitude of flexion in these joints is only 7.6 and 9.4°, respectively. Pronation and supination in the radioelbow joint (42-47°) have a high intensity of change. Sex differences are relatively small.
Table 25. Range of motion in the elbow and shoulder joints 
Table 26. Range of motion in the hip joints 

Let us give a brief analysis of age-related changes in individual joints.
1. The amplitude of flexion of the shoulder joint increases in boys up to 4 years, in girls - up to 6 years. The period of relative stabilization lasts up to 20-29 years. After the age of 40, an ever-increasing decrease in the amplitude of flexion is observed.
2. The amplitude of extension in the shoulder joint increases in both sexes up to 3-6 years, then decreases slightly. A significant decrease in this amplitude begins at the age of 40-59 years.
3. The amplitude of abduction in the shoulder joint increases in both sexes up to 7 years. Until the age of 30-39, a period of relative stabilization continues, and then an ever-increasing decrease in this amplitude begins.
4. The amplitude of rotation of the shoulder outward increases in boys and girls up to 3 years. A relatively stable period lasts up to 30-49 years, and then the mobility progressively decreases.
5. The amplitude of rotation of the shoulder inside increases in both sexes up to 2-3 years. A relatively stable period with a slight decrease in this amplitude lasts up to 30-39 years, and then there is a more significant decrease, especially in old age.
6. The amplitude of flexion in the elbow joint increases in both sexes up to 4 years. The phase of decrease begins from 40-49 years.
7-8. The amplitudes of pronation and supination in the radioelbow joint increase in boys and girls up to 2-3 years. At the same time, at the age of 1-2 years, the amplitude of pronation is greater than the amplitude of supination. In subsequent years, the amplitude of supination decreases to a lesser extent than the amplitude of pronation, as a result of which it significantly exceeds the latter. After 50 years, this difference in both sexes decreases significantly, and in old age the amplitude of pronation again exceeds the amplitude of supination (Fig. 37).

Rice. 37. Age-related changes in the amplitudes of pronation and supination in the radio-elbow joint in males.
1 - supination; 2 - pronation.
9-10. The amplitudes of flexion and extension in the wrist joint increase in both sexes up to 2-3 years. In subsequent years, the extension amplitude decreases to a much greater extent than the flexion amplitude.
11. The amplitude of abduction in the wrist joint increases up to 4 years. The phase of a relatively stable state continues until the age of 50-59; in the elderly and senile age, this amplitude is significantly reduced.
12. The amplitude of adduction in the wrist joint is less than the amplitude of abduction. This amplitude increases in both sexes up to 14-16 years. The phase of decreasing this amplitude begins only in old age (after 60 years).
13-14. Flexion and extension amplitudes in the third metacarpophalangeal joint increase up to 3 years. At this age, the extension amplitude exceeds the flexion amplitude. In subsequent years, the extension amplitude decreases to a much greater extent than the flexion amplitude, especially starting from the age of 17-19. A significant decrease in the amplitude of flexion occurs only after 60 years (Fig. 38).

Rice. 38. Age-related changes in the amplitudes of flexion and extension in the III metacarpophalangeal joint in males.
1 - flexion amplitude; 2 - extension amplitude.
15. The amplitude of flexion in the hip joint with the leg bent at the knee joint increases in boys up to 8-9 years, in girls - up to 5 years. A relatively stable phase continues in both sexes up to 40-49 years. A significant decrease in this amplitude begins after 70 years.
16. The amplitude of flexion in the hip joint with the leg straightened in the knee joint (in the prone position) begins to decrease after a year; a significant decrease occurs after 60 years.
17. The amplitude of extension in the hip joint increases up to 17-19 years, begins to decrease after 40 years.
18-19. The amplitudes of hip rotation outward and inward sharply increase in both sexes up to 3 years. The amplitude of hip rotation outward is greater than inward. The phase of a relatively stable state lasts up to 40-49 years. In the elderly and senile age, a significant decrease in these amplitudes is observed (Fig. 39).

Rice. 39. Age-related changes in the amplitudes of rotation in the hip joint in males.
1 - outward rotation; 2 - rotation inside.
20. Hip abduction amplitude increases up to 5 years. In subsequent years (especially after 40-49 years), this amplitude is significantly reduced.
21. The amplitude of hip adduction increases in both sexes up to 14-19 years. The phase of its decrease begins at the age of 50-59 *.
22. The amplitude of flexion in the knee joint increases in both sexes up to 8-9 years. In subsequent years, there is at first an insignificant, and then, starting from the age of 50-59, an increasingly significant decrease in it.
23-24. Flexion and extension amplitudes in the ankle joint increase up to 3 years. A relatively stable period with a slight decrease in this amplitude lasts up to 30-49 years. At the age of over 70 years, there is a significant decrease in this amplitude.
25-26. The amplitude of adduction in the ankle joint is less than the amplitude of abduction. The increase in the amplitude of adduction lasts up to 2-3 years, the amplitude of abduction - up to 6 years. A significant decrease in these amplitudes begins from the age of 50.
27. The amplitude of pronation-supination mobility in the ankle joint increases up to 3 years. The amplitude of supination is much greater than the amplitude of pronation. With age, there is a significant decrease in these amplitudes, especially after 40-49 years.
On the basis of the variational-statistical analysis of the given material, we developed the norms of the amplitudes of movements in the joints of the extremities for various age and sex groups.
Of great importance is the use of the goniometric method for studying changes in the amplitudes of movements in the joints of the extremities as a result of balneotherapy and functional treatment (physiotherapy exercises) in people with diseases and injuries of the organs of movement. Studies can be performed both before and after individual procedures, and systematically, during the entire course of treatment (for example, every 5 procedures).
Measuring the range of motion in the joints immediately before and after the application of various procedures is important for a comparative analysis of the effectiveness of restoration of mobility as a result of the use of these procedures. Studies show that immediately after the adoption of this procedure, there is an increase in the range of motion in the joints (in relation to the range of motion before the adoption of this procedure). Moreover, at the beginning of the course of treatment, this increase is greater than at the end of its course.
Goniometric studies of the amplitudes of movements in the joints of the extremities, before and after taking sulfur baths and mud applications without and in combination with therapeutic exercises (Pyatigorsk) showed that the restoration of the amplitudes of movements with the complex use of balneotherapy and physiotherapy occurs to a greater extent than with the use of balneotherapy alone . So, for example, as a result of the use of sulfur baths alone without physiotherapy exercises, large values of the dynamics of the amplitudes of movements in the knee joint (more than 8 °) occurred in 5.7% of cases, and in combination with physiotherapy exercises - in 33.4% of cases.
Studies of changes in the amplitudes of movements in the joints of the limbs under the influence of functional treatment (physiotherapy exercises) were carried out by us in the evacuation hospitals of the Sverdlovsk region during the Great Patriotic War (VA Gamburtsev, 1952). The processing of the material of these studies (more than 1000 cases) showed that the restoration of mobility as a result of treatment in its simplest form occurred according to the 2nd order parabola equation. For each type of lesion, it was possible to establish typical average data on the restoration of movements in the joints. This made it possible to more deeply analyze the dynamics of recovery of movements for one or another period of time (Fig. 40).

Rice. 40. Dynamics of amplitudes of movements in the ankle joint under the influence of functional treatment in the hospital.
According to the intensity and timing of the restoration of mobility in the joints, three types of amplitude increase dynamics can be distinguished: with high, medium and low rates of function recovery.
If the rate of recovery of movements according to goniometric studies is low, then it is necessary to change the treatment method. One of the doctor's tasks is to identify and eliminate factors that hinder the recovery of movements.
The analysis of goniometric indicators of restoration of movements in the knee joint with hip fractures as a result of complex treatment shows that the rate of improvement in motor function depends on the location and nature of the injury and the treatment method. In fractures of the middle third of the thigh, in a relatively large percentage of cases, there were types of curves with both high and low recovery rates. In fractures of the lower third of the thigh, types of curves with medium and low recovery rates were observed. The variability of the results in case of damage to the femoral shaft can be explained by the presence, on the one hand, of cases with significant bone destruction over a large area, which required prolonged immobilization, and on the other hand, by the presence of milder injuries.
Here are some examples.
1. Patient A-s. Diagnosis: large-comminuted fracture of the upper preti of the left femur. Entered the evacuation hospital 2 months after the injury. There was a complete lack of mobility in the left knee joint. After 30 days of application of therapeutic exercises, the range of motion in the knee joint reached 45°. Later, due to the complications of osteomyelitis and two sequestrotomies, there was a temporary decrease in mobility. After applying intensive functional treatment, after 3 months of treatment in the hospital, the mobility in the knee joint increased to 70°, after 4 months - up to 90° (the patient began to walk on crutches, stepping on his foot), after 6 months - up to 100° (walked with a stick ), after 6 months - up to 116 °. After 220 days, the patient was discharged to the unit with normal range of motion in the knee joint (140°). Restoration of movements proceeded with average intensity (type 2).
2. Sick Gr-s. Gunshot fracture of the middle third of the right thigh. As a result of active functional treatment, the range of motion increased after 25 days from 20 to 140°. Restoration of movements proceeded with high intensity (type 1).
3. Sick F-s. Fracture of the upper third of the left thigh. As a result of insufficient functional treatment, after 100 days of treatment in the hospital, the range of motion in the knee joint increased from 0 to 40° [low intensity of movement recovery (type 3)]. After applying more intensive functional treatment, the mobility increased after 45 days to 108°.
When peripheral nerves are damaged, a feature of the technique for measuring the amplitudes of active movements is the need to take into account the most insignificant shifts in the restoration of mobility, because they characterize the beginning of nerve regeneration. In addition to measuring the amplitudes of active movements, here, in order to take into account neurogenic contractures, it is necessary to measure the amplitudes of passive movements.
In the practice of work, there were cases when, as a result of insufficient dosage and incorrect selection of treatment agents, the increase in mobility in the joints was insignificant, but as soon as the treatment method was changed, its effectiveness increased significantly.
* The range of motion in the hip joint in children aged 1 to 3 years was studied by R. I. Asfanbiarov (1960).
It is determined in large joints: hip, knee, ankle, shoulder and wrist. For this purpose, the subject is asked to demonstrate the degree of maximum possible flexion and extension in the joints. It should be noted: a) excessive extension ("hypermobility") of the joints, especially the knee and elbow; b) a decrease in the range of motion associated with individual anatomical features, an increase in muscle tone or the consequences of an injury (disease) of the joint; c) "looseness" (instability) of the joint, accompanied by frequent subluxations and dislocations.
The range of motion in a joint is an important indicator in determining the functional ability of a limb. The measurement is carried out using a goniometer, while it is necessary to investigate two types of volume of movement - active and passive (Table 1).
Active volume is the result of the work of the muscles responsible for its implementation.
The passive range of motion is the result of the application of an external force (for example, the hand of a doctor, masseur). As a rule, the passive range of motion is several degrees greater than the active one within physiological limits, however, when measured, it should not be brought to pain.
Table 1
Measurement of range of motion in some joints
Comparison of active and passive ranges of motion allows obtaining additional data, for example, about reflex muscle tension or the lack of providing a full range of motion with the corresponding muscle effort.
ATTENTION!
With pathological changes in the area of the joint under study, the difference between active and passive range of motion can be significant.
Rice. 3. Examination of mobility in the joints (location of branches)
The protractor is applied in such a way that its fixed jaw is located corresponding to the longitudinal axis of the proximal part of the limb (fixed link), and the movable jaw is along the longitudinal axis of the distal part that performs the movement. The proximal part must be sufficiently fixed. Only under these conditions does it become impossible during the study to transfer the movement performed by the adjacent joint (Fig. 3).
The axis of rotation of the goniometer should correspond to the axis of motion of the joint under study (Fig. 4).
Rice. 4. Scheme of angles of motion in the joints:
A) upper limb; b) lower limb
Upper limb
♦ Shoulder joint: a) flexion of the arm is carried out with the help of the deltoid muscle (its front part), the coracobrachialis muscle, the biceps muscle (short head) and the anterior serratus muscle; b) combined movements in the shoulder joint (Table 2).
table 2
Angles of movement in large joints of the limbs (normal)
Abduction of straight arms: arms describe lateral arches in the frontal plane and are connected with palms above the head. The supraspinatus muscle, the deltoid muscle (middle part), and the serratus anterior muscle take part in the execution of this movement.
Definition of internal rotation of the shoulder. The patient should touch his back with his hand (as high as possible) in the interscapular region. This compares the degree of mobility of both shoulders.
Rice. 5. Studies of the range of motion in the shoulder joint
These techniques allow you to determine the relative participation in the movement of the scapula and humerus. The involvement of the scapula can also be determined by the amount of shoulder elevation.
To accurately measure the amplitude of abduction involving the scapular-shoulder joint, it is necessary to fix the scapula. To do this, the doctor (masseur) holds the lower part of the shoulder blade with one hand, and passively and slowly removes the patient's hand with the other. Normal abduction at the scapulohumeral joint is 90°.
Normally, the scapula also participates in the rotation of the shoulder, and this movement is part of the functions of the shoulder, so rotation should be measured by the movement of the entire shoulder girdle. The normal arc of motion is about 90° for internal rotation and 90° for external rotation. The teres minor and infraspinatus muscles participate in external rotation; internal rotation is carried out by the subscapularis, teres major and latissimus dorsi.
♦ Elbow joint. Flexion in the elbow joint is carried out by the biceps brachii, brachioradialis and brachialis muscles. The normal angle between the shoulder and forearm is 160 to 150° from the starting position (0°).
Extension in the elbow joint occurs due to the triceps muscle. The position of full extension at the joint is designated as 0°. Only a few people are 5 or 10 degrees short of full extension, and some have 5 or 10 degrees more extension (Fig. 6).
Rice. 6. study of range of motion in the elbow joint
ATTENTION!
The humeroulnar and humeroradial joints are involved in flexion and extension of the joint.
Pronation and supination of the hand and forearms occur at the proximal and distal radioulnar joints, as well as at the glenohumeral joint. Typically, the range of motion in these joints is almost 180° (about 90° of pronation and about 90° of supination). Supination is carried out due to the arch support of the forearm, and pronation - due to the round and square pronators.
Wrist movements include flexion and extension, radial and ulnar abduction. The combination of these movements is called a circular motion of the wrist. These movements are associated with varying degrees of mobility of the wrist and intercarpal joints. The measurement of the range of motion of the wrist is started with the wrist and hand extended in relation to the forearm (0°). Typically, wrist extension is 70° and flexion is about 80–90° from the starting position (0°). The deviation to the ulnar side averages 50–60° and is almost 20° greater than the deviation to the radial side (Fig. 7).
Rice. 7. Examination of range of motion in the wrist joint
Rice. 8. study of range of motion in the metacarpophalangeal joints (A); in the metacarpophalangeal joint of the first finger (b); at the proximal interphalangeal joint (V); at the distal interphalangeal joint (G); in the interphalangeal joint of the first finger (e)
ATTENTION!
An important functional impairment of wrist mobility is loss or limitation of extension.
Mobility and range of motion of the fingers, including the proximal and distal interphalangeal joints. The mobility of the fingers is first determined as a whole, and then the mobility of each joint is considered separately. The finger function test is a test of the patient's ability to clench the fingers into a fist and fully unbend them. A normally clenched fist, resulting from full flexion of all fingers, is scored as 100%, and an extended palm is scored as 0% of the fist. The metacarpophalangeal joints of the fingers are flexed 90-100°, counting from the normal average position during extension (0°). However, the metacarpophalangeal joint of the first finger is only flexed by 50°. The proximal interphalangeal joints are flexed by 100–120°, and the distal ones by 45–90°, counting from the initial extended position (0°).
> At the metacarpophalangeal joint, hyperextension of almost 30° is possible. At the same time, in the proximal interphalangeal joint, hyperextension is possible by no more than 10°, and in the distal joint, on the contrary, by more than 30°.
> Each finger can be abducted (spreading the fingers of the entire hand) and adducted (move the fingers towards the third finger) with extended metacarpophalangeal joints. The total amount of adduction-abduction in the metacarpophalangeal joint is about 30–40°, but the degree of adduction and abduction varies from joint to joint (Fig. 8).
lower limb
hip joint has great mobility. Flexion, extension, adduction, abduction, rotation are possible in it. The angle between the femoral neck and the diaphysis partially transforms angular movements - flexion, extension, adduction, abduction into rotational movements of the femoral head in the articular cavity.
Hyperextension is examined in the initial position (ip) of the patient lying on his stomach, the doctor fixes the pelvis with one hand, and raises the patient's leg with the other. Normal hip hyperextension is 15° if the leg is straight and the pelvis and spine are immobile.
The greatest degree of hip flexion is obtained when the leg is bent at the knee joint. The hip can be flexed almost 120° from the middle or extended position (0° or 180°) if the limb was previously bent at the knee joint to 90°, and held in this position by a doctor (masseur). With a straight leg, the tension of the hamstrings limits the flexion in the hip joint so that the angle between the thigh and the long axis of the body will be no more than 90 °.
Lead and adduction are examined in I.P. patient lying on his back, legs straight. Measure the angle between the imaginary midline, which serves as a continuation of the longitudinal axis of the body, and the longitudinal axis of the leg. The degree of abduction increases, it is combined with flexion and decreases when combined with extension in the hip joint. The normal volume of abduction in the hip joints with straight legs is 40–45° and is limited by the puboccapsular ligament and the middle portions of the iliac-femoral ligaments.
ATTENTION!
Abduction can be inhibited by spasm of the adductor muscles in a healthy joint.
Adduction of straight legs is limited by the fact that the legs touch one another, but adduction with flexion at the hip joint, allowing you to cross your legs, gives a span of 20-30 ° from the average (initial) position.
Normal rotation in the hip joint is about 45° outward and about 40° inward. Outward rotation is limited by the lateral bundle of the iliofemoral ligament, and inward rotation by the ischiocapsular ligament. The amount of rotation in the hip joint increases with flexion and decreases with extension at this joint.
ATTENTION!
Restriction of internal rotation is the earliest sign of joint damage.
Knee-joint. Normally, the extended limb can form a straight line (0° or 180°), and in some cases increase by an additional 15°. The extension angle is measured between the thigh and lower leg. Then measure the volume of active or passive flexion of the lower leg. Normally, this volume is from 135° to 150°. A simple but less accurate way to determine the angle of flexion is by the distance between the heel and the buttock when the legs are maximally bent at the knee joints (Fig. 10).
Rice. eleven. Examination of range of motion in the ankle joint
♦ Pronation and supination of the foot usually occur in the subtalar joint. With supination, the foot is turned with the sole inward, and with pronation, it is turned outward. The subtalar joint can pronate 20° and supinate 30° from the normal resting position (Fig. 12).
♦ At the metatarsophalangeal joint I finger extension is possible at 80 ° and flexion - at 35 °. In the metatarsophalangeal joints of the remaining fingers, the flexion-extension range is 40° (Fig. 13).
Rice. 14. Examination of range of motion in the proximal joints of the foot
Examination of the cervical region should begin with determining the volume of passive and active movements. Normally, flexion-extension is possible within 130–160°, turn to the side - 80–90°, and tilt (ear to shoulder) - up to 45°. In order to determine whether the tilt of the head is limited as a result of damage to the upper cervical or craniovertebral level, the upper cervical region is fixed with one hand, and the head is tilted with the other. With passive and active tilts aimed at stretching certain muscle groups (when tilting to the right - left muscles, etc.), the so-called cervical symptom of Lasegue occurs. Then, the response to stretching of all tissues of the neck is determined. To do this, you need to stand behind the patient, press your palms to his lower jaws so that they can be pulled up with the surfaces of the third fingers. The pads of the thumbs are pressed against the back of the head, slightly bending the patient's head. Raising with a slight effort their palms with the patient's lower jaw up, they slightly stretch all the tissues of the neck.
The total volume of flexion of the spine is 160° (cervical - 70°, thoracic - 50° and lumbar - 40°), extension - respectively 60°, 55° and 30°, lateral tilt - 30°, 100° and 35°, rotation – 75°, 40° and 5° (M.F. Ivanitsky).
In the anatomy of the upper limbs, the joints of the shoulder girdle and the free part of the arm are considered separately. All bones are connected to each other with the help of joints, they provide the mobility of the limbs. Also, the joints of the upper limbs include reinforcing, inhibitory and guiding ligaments, which are dense strands that are formed by connective tissue.
The formation of limbs in phylogenesis is associated with a change in the habitat and the exit of vertebrates from the aquatic environment to land. Movement on the surface of the Earth required the development of a system of "levers" that allow locomotion (movement of the body in space) on land under the constant action of the force of the Earth's gravitational field on the body.
In most terrestrial vertebrates, the fore and hind limbs have a homologous (similar) structure and consist of a limb belt, with which it is fixed relative to the body skeleton, and a free part of the limb, consisting of three main segments: proximal, middle and distal (five-fingered), which connected to each other by movable joints.
The mobility of the arm is mainly determined by movements in its main joints, connecting the main segments of the upper limb: the shoulder, forearm and hand, and also connecting it to the trunk.
The main connections of the skeleton of the human upper limbs are described in detail in this material.
Connections of the shoulder girdle of the upper limbs
sternoclavicular joint ( articulatio sternoclavicularis) plays a key role in the mobility of the shoulder girdle, and with it the entire arm. It is formed by the clavicular notch (incisura clavicularis) of the sternum and the sternal articular surface (facies articularis sternalis) of the clavicle. The joint is saddle-shaped.
joint capsule ( capsula articularis) attached along the edge of the articular surfaces and relatively free. Outside, it is strengthened by ligaments: anterior and posterior sternoclavicular, interclavicular and costoclavicular, which somewhat limit the freedom of movement in this joint.
In the cavity of this joint of the belt of the upper limb is articular disc ( discus articularis) , which, with its edges, is fused with the articular capsule; as a result of this, the joint cavity is divided into two sections.
The presence of intra-articular cartilage allows movement in this joint as in a multiaxial one. When raising and lowering the shoulder girdle, the rotation of the clavicle occurs around the sagittal axis; when the shoulder girdle moves forward and backward, the clavicle rotates around a vertical axis. Finally, a circular movement of the clavicle along with the shoulder girdle is possible according to the type of circumduction.
The connection of such bones of the upper limbs as the scapula and collarbone is performed using a sedentary acromioclavicular joint ( articulatio asgo-mioclavicularis) formed between the acromion and the acromial end of the clavicle. This is a simple flat-shaped joint, the articular capsule of which is tightly stretched and strengthened. acromioclavicular ligament ( lig. acromioclaviculare) .
In addition, the articulation of the scapula with the clavicle is held by a powerful coracoclavicular ligament ( lig. coracoclaviculare) , consisting of two bundles: the trapezoid ligament, lying laterally, and the cone-shaped ligament, located medially. As a result, the scapula moves relative to the body along with the collarbone; when changing the position of the shoulder girdle, the main movements occur in the sternoclavicular joint.
Among the syndesmoses of the scapula, a significant functional role is played by coracoacromial ligament ( lig. coracoacromiale) - a strong broad ligament stretched between the coracoid and humeral (acromion) process of the scapula above the shoulder joint. It limits the movement in the shoulder joint when the arm is abducted.
shoulder joint ( articulatio humeri) - the main joint of the upper limb, which ensures the mobility of the entire arm relative to the shoulder girdle. He is educated articular cavity ( cavitas glenoidalis) scapula and head of the humerus ( caput-humeri) . The articular cavity is much smaller than the surface of the head of the humerus, which provides a large range of motion in the shoulder joint.
For greater congruence of the articular surfaces (i.e., for better matching of their curvature) in this joint, the hyaline cartilage covering the articular cavity is supplemented along its edge cartilaginous lip ( iabrum glenoidale) . The joint is simple, spherical in shape.
The joint capsule is thin, free, attached along the bony edge of the articular cavity of the scapula and along the anatomical neck of the humerus. From above, it is reinforced with a fibrous cord in the form of a coracohumeral ligament (lig. coracohumerale), which goes from the base of the coracoid process of the scapula and is attached to the large tubercle of the humerus; this ligament of the humeral joint of the upper limb holds the bones in an articular state and limits the adduction of the shoulder and its supination.
The synovial membrane of the capsule has outgrowths: intertubercular synovial sheath ( vagina synovialis intertubercularis) , which covers the tendon of the long head of the biceps muscle of the shoulder, which lies in the intertubercular groove of the humerus, passes through the joint cavity and is attached to the supraarticular tubercle; subtendinous bursa (bursa subtendinea) of the subscapularis muscle, located at the base of the coracoid process.
 The shoulder joint of the skeleton of the upper limb is the most mobile of all joints; it is a multiaxial joint. Movements in it occur around the transverse axis - flexion and extension, the sagittal axis - abduction and adduction, and the vertical axis - rotation inwards (pronation) and outwards (supination). Perhaps a circular motion - circumduction.
The shoulder joint of the skeleton of the upper limb is the most mobile of all joints; it is a multiaxial joint. Movements in it occur around the transverse axis - flexion and extension, the sagittal axis - abduction and adduction, and the vertical axis - rotation inwards (pronation) and outwards (supination). Perhaps a circular motion - circumduction.
Abduction in the shoulder joint is limited by the coracoid-acromial ligament stretched between the processes of the same name of the scapula. This connection of the bones of the girdle of the upper limb limits the abduction of the arm to an angle of 80-90 °, since in this position the humerus, with its large tubercle, rests against the coracoid-acromial ligament. Further raising of the arm is carried out already due to movement in the sternoclavicular joint.
Connections of the free part of the upper limb: elbow joint
elbow joint ( articulatio cubiti) The upper limb is made up of three bones: the humerus, ulna, and radius.
This is a complex joint, since three joints are formed between the bones, enclosed in one joint capsule.
- shoulder joint ( art. humeroulnaris) - formed by a block of the humerus and block-shaped notch of the ulna; the joint is blocky in shape;
- shoulder joint ( art. humeroradialis) - formed by the head of the condyle of the humerus and the head of the radius; the joint is spherical in shape, but with limited movements;
- Proximal radioulnar joint ( art. radioulnaris proximalis) - formed by the radial notch of the ulna and the articular circumference of the head of the radius; This joint is cylindrical in shape.
The articular capsule of the elbow joint is free, attached along the edge of the articular surface on the ulna, the neck of the radius and above the edge of the articular surfaces on the humerus.
On the sides, the joint capsule is reinforced with fibrous cords in the form of the following ligaments:
- Ulnar collateral ligament ( lig. collaterale ulnare) upper limb, which starts from the medial epicondyle of the shoulder and is attached along the edge of the trochlear notch;
- Radial collateral ligament ( lig. collateral radiale) - starts from the lateral epicondyle of the shoulder, approaches the articular circumference of the radius, at the level of which it is divided into two fibrous bundles. These bundles cover the head of the radius anteriorly and posteriorly and attach to the radial notch, forming annular ligament of the radius ( lig. anulare radii) , which firmly holds it in the joint.
The main movement in the elbow joint - flexion and extension - is carried out around the transverse axis. In addition, with combined movements in the proximal and distal radioulnar joints, pronation (movement of the distal part of the arm, in which the palmar surface turns inward) and supination (turning the palmar surface outward), which occur around the vertical axis, occur in the elbow joint.
Connection of the bones of the forearm of the upper limb
The interosseous edges of the bones of the forearm are connected interosseous membrane of the forearm ( membrana interossea antebrachii) .
Distal radioulnar joint ( articulatio radioulnaris distalis) of the free part of the upper limb - formed by the articular surface of the head of the ulna and the ulnar notch of the radius, supplemented by a triangular articular disc, whose upper surface faces the ulna. The joint is cylindrical in shape.
The distal and proximal radioulnar joints of the human upper limbs form a combined joint, in which rotational movements occur around the vertical axis - pronation and supination.
wrist joint ( articulatio radiocarpalis) - a complex joint that provides mobility to the distal segment of the arm - hand.
It is formed by the carpal articular surface of the radius and the first row of carpal bones, which together form an elliptical-shaped common articular surface.
articular disc ( discus articularis) separates the head of the ulna, which is involved in the formation of the distal radioulnar joint, from contact with the bones of the wrist and complements the carpal articular surface of the radius.
The articular capsule is attached along the edge of the surfaces of the joints of the bones of the upper limb and along the outer edge of the articular disc. It is reinforced on all sides with ligaments; This radial And ulnar collateral ligaments of the wrist ( ligg. collateralia carpi radiate and ulnare) , palmar wrist And dorsal radiocarpal ligament ( ligg. radiocarpea palmare et dorsale) , and radiate ligament of the wrist ( lig. carpi radiatum) - dense fibrous bundles going from the head of the capitate to the nearby bones of the wrist.
These ligaments hold the bones in place and limit the range of motion.
In the wrist joint, movements occur around two axes: flexion and extension (around the transverse axis), abduction and adduction of the hand (around the sagittal axis), as well as circular movement of the hand - circumduction.
Connection of the bones of the hand of the upper limb
There are many movable joints on the hand, especially on the fingers, which ensures a firm grip of the object and its retention due to the opposition of the thumb
Between the bones of the wrist and metacarpus there are many small, inactive joints. Among them are distinguished intercarpal joints ( articulationes intercarpales) , which are formed by the articular surfaces of the bones of the wrist facing each other; mid-carpal joint ( articulatio mediocarpalis) - between the bones of the proximal and distal rows of the bones of the wrist.
 There are practically no movements in these joints of the free upper limb. The joints are reinforced with ligaments: intracarpal interosseous, intercarpal palmar and dorsal.
There are practically no movements in these joints of the free upper limb. The joints are reinforced with ligaments: intracarpal interosseous, intercarpal palmar and dorsal.
carpometacarpal joints ( articulationes carpometacarpales) - flat, formed by the distal row of carpal bones and the bases of the metacarpal bones. The articular capsule is attached along the edge of the articular surfaces, strengthened by tightly stretched ligaments: palmar and dorsal carpometacarpal. There is practically no movement in the joints.
Intercarpal joints ( articulationes intermetacarpales) formed by the articular surfaces of the bases of the II-V metacarpal bones facing each other. The articular capsules are reinforced by interosseous, palmar and dorsal metacarpal ligaments. There is practically no movement in the joints.
The distal row of the bones of the wrist, as well as the II-V metacarpal bone, interconnected by means of inactive joints and strengthened by numerous syndesmoses, are designated as a solid base of the hand.
of great functional importance carpometacarpal joint of the thumb ( articulatio carpometacarpalis pollicis) . This is a simple joint formed by the trapezoid bone and the base of the I metacarpal bone. The joint is saddle-shaped. The articular capsule is free, attached along the edge of the articular surfaces. Due to the saddle shape of this joint, along with abduction and adduction, opposition (oppositio) of the thumb to all others is possible, which contributes to the capture of objects with the brush and their strong holding.
 metacarpophalangeal joints ( articulationes metacarpeophalangeae)
. Each joint is formed by the head of the metacarpal bone and the base of the proximal phalanx. The heads of the II-V metacarpal bones are interconnected by ligaments. The articular capsule is free, strengthened by ligaments: lateral collateral ligaments and palmar ligament. In shape, these joints of the bones of the free upper limb are close to ellipsoidal.
metacarpophalangeal joints ( articulationes metacarpeophalangeae)
. Each joint is formed by the head of the metacarpal bone and the base of the proximal phalanx. The heads of the II-V metacarpal bones are interconnected by ligaments. The articular capsule is free, strengthened by ligaments: lateral collateral ligaments and palmar ligament. In shape, these joints of the bones of the free upper limb are close to ellipsoidal.
Movements in the joints occur around the sagittal axis - abduction and adduction, around the transverse axis - flexion and extension; possible circular movements of the fingers. In the metacarpophalangeal joint of the thumb, two sesamoid bones are enclosed in the articular capsule on the palmar side. Movement in it is possible only around the transverse axis - flexion and extension.
Interphalangeal joints of the hand ( articulationes interphalangeae manus) formed by the heads of the proximal phalanges and the bases of the middle phalanges, as well as the heads of the middle phalanges and the bases of the distal phalanges. In shape, these are block-shaped joints.
The articular capsule is attached along the edge of the articular surfaces, it is strengthened collateral ( ligg. collateralia) And palmar ligaments ( ligg. palmaria) . In the interphalangeal joints, only flexion and extension occurring around the transverse axis is possible. Due to the bending of the phalanges relative to each other, the girth of the object is achieved.
Differences in the joints of the upper and lower limbs
In humans, in the process of evolution, movement in an upright position on two legs was formed. In this regard, there was a differentiation of the limbs into the upper one - the arm (an organ for studying the environment and the organ of labor) and the lower one - the leg (the organ of movement). The hand, as an organ of labor, requires great mobility in all major joints, the ability to grasp objects, and fine and precise finger movements.
 The lower limbs, the main function of which is to support the body and move it in space, are adapted for their implementation by limiting mobility in the joints and the formation of special anatomical structures that provide cushioning of the body during shocks while walking.
The lower limbs, the main function of which is to support the body and move it in space, are adapted for their implementation by limiting mobility in the joints and the formation of special anatomical structures that provide cushioning of the body during shocks while walking.
When comparing the structure of the belts of the upper and lower extremities, it is obvious that, due to the significant mobility, the shoulder girdle, consisting of the clavicle and scapula, has a very mobile connection with the skeleton of the body.
Useful articles
With a general similarity in the structure of the skeleton of both limbs, there are significant differences between them, which are due to the difference in functions. To some extent, these differences are inherent in the entire class of mammals, in most of whose representatives the pelvic limbs play the role of the main motor (for example, repulsion when jumping), and the thoracic limbs, along with support and locomotion, are used for grasping food and other behavioral reactions. Therefore, the joints of the thoracic limb, as a rule, have greater mobility, and the joints of the pelvic limb are characterized by stability. Suffice it to recall that the thoracic limb is connected to the body through two movable bone links - the clavicle and scapula, while the girdle of the pelvic limbs in most mammals is a closed, immovable bone ring.
The evolution of the limb skeleton in primates is associated with the development of a grasping function, which occurred due to an increase in the mobility of the fingers, especially the first toes of the hand and foot. The forelimbs in primates have acquired more diverse functions as organs for the study of objects. With their help, animals collect food and bring it to their mouths, and higher primates manipulate objects. In this regard, the forelimbs in primates are more adapted to a variety of movements than in other mammals.
In humans, differences in the structure and function of the upper and lower extremities are even more pronounced. Thanks to upright posture, the hand was freed from the function of support and movement and became a specialized organ of labor, and also acquired the ability to fine touch. The lower limb has lost its grasping function and has become the main organ of support and locomotion. This determines the structural features of the joints and ligamentous apparatus of the upper and lower extremities.
The shoulder girdle is connected to the sternum through the sternoclavicular joint, which contains the articular disc in its cavity. The joint resembles to a certain extent a spherical joint, but its surfaces are saddle-shaped. However, due to the presence of a disk, movements in this joint are made around 3 axes. Consequently, it only in function approaches the spherical, triaxial, but with a limited range of motion.
Between the scapula and the clavicle is the acromioclavicular joint with ellipsoidal surfaces; it provides additional mobility of the shoulder girdle after the range of motion in the sternoclavicular joint has already been exhausted. In 1/3 of cases, the articular disc is found in the joint cavity. In the acromioclavicular joint, movements around three axes are possible, but their amplitude is insignificant.
The ligaments that strengthen these joints do little to restrict movement and, at the same time, participate in the transmission of forces from the free limb to the scapula and collarbone and through the latter to the sternum. The coracoclavicular ligament plays a particularly important role in holding the bones of the shoulder girdle together. When the acromioclavicular joint closes, this ligament is tensed, and the scapular-clavicular complex moves as a whole.
The shoulder joint is the most "free" of the large joints of the human body. Movements around all three axes can take place here on a large scale. The mobility of the joint is achieved due to its stability and reliability. The joint capsule is weakly strengthened by ligaments, and the muscles play a large role in strengthening the shoulder joint. The shoulder joint has a number of morphological features:
1. Incongruence of the articular surfaces - the surface of the head of the humerus is almost 3 times the surface of the articular cavity of the scapula. Therefore, the cavity is supplemented by the articular lip.
2. Intra-articular course of the tendon of the long head of the biceps brachii.
3. The arch of the joint, consisting of the acromion and the coracoid process of the scapula and the coracoid-acromial ligament.
The joint has a rather loose capsule, strengthened in the upper part by only one ligament, the coracohumeral ligament, which is a thickened section of the joint capsule. In general, the shoulder joint does not have real ligaments and is strengthened by the muscles of the shoulder girdle.
The synovial membrane forms two extra-articular protrusions: the intertubercular synovial sheath surrounding the tendon of the long head of the biceps brachii muscle, and the tendon bag of the subscapularis muscle, located at the base of the coracoid process of the scapula. Movements in the joint are carried out around 3 axes and circular motion is possible. However, flexion and abduction in the joint is possible only to a horizontal level, since these movements are inhibited by the abutment of the large tubercle of the humerus against the coracoacromial ligament.
Movements in the shoulder joint and joints of the shoulder girdle are usually performed together. When the arm is raised to a horizontal level, the clavicle is raised and rotated around its own longitudinal axis. Movements of the upper limb above the horizontal level are made in the sternoclavicular joint when the clavicle is raised together with the free upper limb, and the scapula makes a turn with the displacement of its lower angle forward and laterally. Therefore, functionally, the shoulder joint is closely related to the joints of the scapula and clavicle, so they are combined under the name of the shoulder complex.
The elbow joint contains 3 joints in one capsule: humeroulnar, humeroradial and proximal radioulnar. Therefore, in its structure, the elbow joint belongs to complex joints.
The shoulder-elbow joint is a block-like articulation with a helical structure of the articular surfaces with a frontal axis of rotation.
The shoulder joint is spherical in shape, but in fact, movements in it are made only around two axes (vertical and frontal), since the ulna limits movement.
The proximal radioulnar joint has a cylindrical shape with a vertical axis of rotation and is combined with the distal radioulnar joint.
The elbow joint is inferior to the knee joint in terms of the number of degrees of freedom, as if violating the rule of greater mobility of the joints of the upper limb, however, this concession is fully compensated by the radioulnar joints. Movements in the elbow joint are of two kinds. Firstly, flexion and extension of the forearm around the frontal axis in the humeroulnar joint takes place in it, and the radius also moves. The range of motion around the frontal axis is 140°. Secondly, the rotation of the radius around the vertical axis in the glenohumeral joint, as well as in the proximal and distal radioulnar joints. Since the brush is connected with the lower end of the radius, the latter follows the radius when moving. The movement in which the rotating radius crosses the ulna at an angle, and the hand turns with the back side forward (with the arm lowered), is called pronation. The opposite movement, in which both bones of the forearm are parallel to each other, and the hand is turned with the palmar side forward, is called supination. The range of motion during supination and pronation is about 140°. The ability to pronation - supination gives the brush an additional degree of freedom in movement.
The bones of the forearm are connected to each other by means of continuous and discontinuous connections. Continuous connections include the interosseous membrane of the forearm, which connects the diaphysis of the ulna and radius bones. Discontinuous connections of the bones of the forearm are the proximal and distal radioulnar joints, which form a combined cylindrical joint with a vertical axis of rotation. The volume of rotation in the radioulnar joints is about 180°. If at the same time the shoulder and scapula make an excursion, then the hand can turn almost 360 °. The rotation of the radius is unimpeded in any position of the ulna: from the extended state to full flexion.
The wrist joint is formed by the distal end of the radius, the articular disc stretched between the ulnar notch of the radius and the styloid process of the ulna, and the proximal row of the carpal bones: scaphoid, lunate and triquetrum. Consequently, the ulna participates in the wrist joint only through the cartilaginous disc, not having a direct relation to this articulation. In its structure, the wrist joint is complex, and in the shape of the articular surfaces it is ellipsoid with two axes of rotation - frontal and sagittal. The joint is strengthened by 4 ligaments, which are located, as it were, at the ends of the axes of rotation:
1) radial collateral ligament of the wrist, which inhibits the abduction of the hand,
3) palmar radiocarpal ligament, which limits flexion,
4) dorsal radiocarpal ligament, which limits extension.
The joint is functionally connected with the nearest joints of the hand.
The mid-carpal joint is located between the proximal and distal row of carpal bones and is functionally connected to the radiocarpal joint. Articulating surfaces have a complex configuration, and the joint space is S-shaped. Thus, in the joint there are, as it were, 2 heads, one of which is formed by the navicular bone, and the second by the capitate and hamate bones. The first articulates with the trapezoid bone and the trapezius bone, and the second with the trihedral, lunate and scaphoid bones. The cavity of the midcarpal joint connects with the cavities of the intercarpal joints. Movement in this joint is possible only around the frontal axis.
The intercarpal joints are flat in the shape of the articular surfaces, strengthened by the palmar and dorsal intercarpal ligaments, interosseous intercarpal ligaments, and the radiant ligament of the wrist. The relative independence of the navicular bone, which functionally belongs to the thumb, is noted.
The carpometacarpal joints are formed by the distal articular surfaces of the second row of carpal bones and the articular surfaces of the bases of the metacarpal bones.
The carpometacarpal joint of the thumb differs in shape from the rest and is a typical saddle joint with a large range of motion. It is completely isolated from other carpometacarpal joints. Movement in it occurs around 2 axes: frontal (apposition and reposition) and sagittal (abduction and adduction). Circular motion is also possible in this joint. The range of motion is 45-60° in abduction and adduction and 35-40° in apposition and reposition.
The carpometacarpal joints of the II - V fingers have a common articular cavity and are strengthened by the dorsal and palmar carpometacarpal ligaments. In shape, these joints are flat, stiff. They can slip by 5-10°.
The metacarpal joints are formed by the surfaces of II - V metacarpal bones adjacent to each other. The capsule of these joints is common with the capsule of the carpometacarpal joints. The shape of the joints is flat, stiff.
In the movements of the hand relative to the forearm, the wrist, middle wrist, carpometacarpal statutes, as well as the intercarpal and intercarpal joints take part.
All these joints, united by a single function, are often called the wrist joint by clinicians. The complex of connections between the radius and the bones of the wrist as a whole (the wrist joint) allows a wide range of motion comparable to that of the shoulder joint. The total range of motion of the hand is the sum of the motions in all these joints. The range of motion simultaneously in the wrist and mid-carpal joints during flexion is 75-80°, during extension - about 45°, during abduction - 15-20°, during adduction - 30-40°.The carpometacarpal, intercarpal and intercarpal joints are reinforced by strong and tightly stretched ligaments, and therefore have extremely little mobility. Therefore, from can be attributed to amphiarthrosis. The bones of the second row of the wrist, which are firmly connected to each other and to the II - V metacarpal bones, mechanically constitute a single whole - the solid base of the hand.
The metacarpophalangeal joints are spherical in shape of the articular surfaces, however, movement in them is possible around 2 axes - frontal and sagittal, and circular movement. Range of motion during flexion and extension - 90-100°, during abduction and adduction - 45-50°. Abduction and adduction is possible only with extended fingers, when the collateral ligaments that strengthen these joints are relaxed.
Interphalangeal joints in the form of articular surfaces are typical block-shaped with a frontal axis of rotation. The total range of motion is about 90°.
lower limb
In contrast to the shoulder girdle, the bones of the girdle of the lower limb are more firmly connected. The sacroiliac joint, in terms of the shape of the articular surfaces, belongs to flat joints, but due to the presence of strong ligaments and the congruence of the articulating surfaces, the movements in it are insignificant. Therefore, it is referred to as "tight" joints, amphiarthrosis. A slight mobility of this joint persists until puberty, and in women and in adulthood. The spine and pelvic bone can move away from each other like the leaves of a sliding door and rotate in the anteroposterior direction and back.
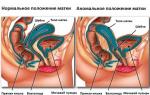
The pelvic bones and the sacrum, connecting with the help of the sacroiliac joint and the pubic symphysis, form the pelvis. The pelvis is a bony ring, inside of which there is a cavity containing the insides. The pelvic bones with the iliac wings deployed to the sides provide a reliable support for the spinal column and abdominal viscera. The pelvis is divided into 2 sections: the large pelvis and the small pelvis. The boundary between them is the boundary line.
The large pelvis is bounded behind by the body of the V lumbar vertebra, on the sides by the wings of the ilium. In front, a large pelvis has no walls.
The small pelvis is a narrowed downward bone canal. The upper aperture of the small pelvis is limited by the boundary line, and the lower aperture (exit from the small pelvis) is limited behind by the coccyx, on the sides by the sacrotuberous ligaments, ischial tuberosities, branches of the ischial bones, lower branches of the pubic bones, and in front by the pubic symphysis. The posterior wall of the small pelvis is formed by the sacrum and coccyx, the anterior - by the lower and upper branches of the pubic bones and the pubic symphysis. From the sides, the cavity of the small pelvis is limited by the inner surface of the pelvic bones below the border line, the sacrotuberous and sacrospinous ligaments. On the side wall of the small pelvis are the large and small sciatic foramen.
In the vertical position of the human body, the upper aperture of the pelvis is tilted anteriorly and downwards, forming an acute angle with the horizontal plane: in women - 55-60 °, in men - 50-55 °.
In the structure of the pelvis of an adult, sexual characteristics are clearly expressed. The pelvis in women is lower and wider than in men. The distance between the spines and iliac crests in women is greater, since the wings of the iliac bones are more deployed to the sides. The cape in women protrudes less than in men, so the upper aperture of the female pelvis has a more rounded shape. The angle of convergence of the lower branches of the pubic bones in women is 90-100°, and in men - 70-75°. The pelvic cavity in men has a pronounced funnel-shaped shape, in women the pelvic cavity approaches the cylinder. In men, the pelvis is taller and narrower, while in women it is wider and shorter.
For the birth process, the size and shape of the pelvis are of great importance. Knowing the size of the pelvis is necessary to predict the course of labor.
When measuring the large pelvis, 3 sizes are determined:
1. The distance between the two anterior superior iliac spines (distantia spinarum) is 25-27 cm.
2. The distance between the iliac crests (distantia cristarum) - 28-29 cm.
3. The distance between the large skewers of the femur (distantia trochanterica) - 30-32 cm.
When measuring the small pelvis, the following dimensions are determined:
1. Outer direct size - the distance from the symphysis to the depression between the V lumbar and I sacral vertebrae - 20-21 cm. symphysis) subtract 9.5-10 cm, get 11 cm.
2. The distance between the anterior-superior and posterior-superior iliac spines (lateral conjugate) - 14.5-15 cm.
3. To determine the transverse size of the entrance to the small pelvis (13.5-15 cm), divide distantia cristarum in half or subtract 14-15 cm from it.
4. The size of the exit from the small pelvis - the distance between the inner edges of the ischial tuberosities (9.5 cm) plus 1.5 cm for the thickness of the soft tissues - only 11 cm.
5. The direct size of the exit from the small pelvis is the distance between the coccyx and the lower edge of the symphysis (12-12.5 cm) and minus 1.5 cm for the thickness of the sacrum and soft tissues - only 9-11 cm.
The hip joint in the shape of the articular surfaces is cup-shaped and has 3 degrees of freedom. In the joint cavity there is a ligament of the femoral head and along the edge of the acetabulum - the articular lip. The range of motion in the joint is much less than in the shoulder joint, especially in extension (about 19°) and adduction. The limiter of movements is a powerful ligamentous apparatus. The iliac-femoral ligament plays a particularly important role in strengthening the joint, which prevents the body from tipping back when it is in a straightened position. It is shown that the lower part of this ligament can withstand a load of up to 100 kg, and the lateral part - up to 250 kg. The pubofemoral ligament delays abduction and inhibits outward rotation. The sciatic-femoral ligament delays the internal rotation of the thigh and inhibits adduction. Movements in the hip joint are usually combined; flexion is combined with abduction and external rotation, and extension is accompanied by adduction and internal rotation. The amount of flexion depends on the position of the knee joint. The greatest flexion (118-121°) is possible with the lower leg bent at the knee joint. If the knee joint is extended, then the tension of the muscles on the back of the thigh inhibits flexion, and its volume is 84-87 °. The volume of rotation is 40-50°, the volume of abduction is 70-75°.
Three bones are involved in the formation of the knee joint: the femur, tibia and patella. There are 2 intra-articular (cruciate) ligaments and 2 menisci in the joint cavity. Hence, the joint is complex and complex. The knee joint in the form of articular surfaces is condylar, movements are possible around the frontal and vertical axes. Near the joint lie several synovial bags, some of which communicate with the joint cavity. On the anterior surface of the patella - subcutaneous, subfascial, tendon prepatellar bags, between the tendon of the quadriceps femoris and the femur - the suprapatellar bag, between the patellar ligament and the tibia - a deep subpatellar bag. In the posterior region of the joint, the bursae meet under the insertions of almost all muscles.
The shape of the condyles of the femur, the spiral curvature of the articular surfaces are important for movements that combine sliding and rotation. The movements involve the menisci and cruciate ligaments. The latter not only limit, but also direct the movements of the joint. Characteristic of movement in the knee joint is the outward rotation of the femur in the initial phase of flexion, opening the joint. At the end of extension, the femur rotates inward, which contributes to the closure of the joint. The stability of the knee joint cannot be achieved by bones and ligaments, the surrounding muscles are also of great importance. In a position with bent lower limbs, the muscles show their stabilizing function to the greatest extent. The total volume of flexion and extension is 140-160°, and the cruciate ligaments and tendon of the quadriceps femoris slow down the flexion. Due to the relaxation of the collateral ligaments during flexion in the knee joint, rotation is possible. The total volume of active rotation is about 15°, passive - 30-35°. The cruciate ligaments inhibit and limit inward rotation, while outward rotation is limited by tension in the collateral ligaments. During extension in the knee joint, the thigh and lower leg are located on the same line, and the cruciate and collateral ligaments are strongly stretched, and the condyles of the thigh rest against the proximal epiphysis of the tibia. In this position, the joint closes, and the lower leg and thigh form a fixed support.
The joints of the bones of the lower leg, unlike the joints of the bones of the forearm, are inactive. The bones of the lower leg are connected to each other proximally through a flat joint with a very limited range of motion, and distally through syndesmosis. The diaphyses of the bones are connected by the interosseous membrane of the leg. With a fixed foot, only slight rotation of the fibula around the tibia can occur. The tibiofibular joint connecting these bones is considered to be flat, however, special studies have shown that the shape of the surfaces in the tibiofibular joint is variable; the surface on the tibia is usually convex, and the surface on the fibula is correspondingly concave.
The ankle joint is a typical trochlear joint. In the ankle joint, movement around the frontal axis is possible - flexion and extension - with a total volume of 60-70 °. When flexing, small movements to the sides are possible, since in this case the narrowest part of the talus block enters the widest part between the ankle bones of the lower leg. The ankle joint during movements is combined with the subtalar; the latter provides a parallel and stable connection of the talus and calcaneus.
In the joints of the bones of the tarsus, 4 joints are distinguished.
- The subtalar joint is cylindrical, with a sagittal axis of rotation.
- Talon-heel-navicular - spherical. Movements in this joint are carried out in conjunction with movements in the subtalar joint, that is, both joints function as a combined joint.
- The calcaneocuboid is saddle-shaped, however, the movements are limited and only a slight rotation around the sagittal axis is possible, which complements the movements in the talocalcaneo-navicular joint. The calcaneocuboid joint, together with the adjacent talonavicular joint (part of the talocalcaneocavicular joint), is described as the transverse tarsal joint (Chopard's joint). In addition to the ligaments that strengthen each joint separately, there is a common ligament for these two joints - a bifurcated ligament. When dissecting this ligament, the transverse joint of the tarsus is easily dissected. Therefore, the bifurcated ligament is called the key of Choparov's joint.
- Wedge-navicular - flat, inactive.
Movement in the joints of the tarsus is carried out around the sagittal axis - adduction and abduction, and this axis goes obliquely, entering on the back side into the head of the talus and exiting from the side of the sole on the lateral surface of the calcaneus. The talus at the same time remains motionless, and together with the calcaneus and navicular bones, the entire foot moves. During adduction (outward rotation), the medial edge of the foot rises, and its back surface turns laterally (supination). During abduction (inward rotation), the lateral edge rises and the dorsal surface rotates medially (pronation). The total range of motion does not exceed 55°. In addition, movement around the vertical axis is possible here, when the tip of the foot deviates medially and laterally from the midline. Finally, there may be extension and flexion around the frontal axis. Vertical movements of the bones are also possible, which increase the springy properties of the leg. All these movements are small and usually combined.
The tarsus-metatarsal joints are flat, movements in them are minimal. For practical reasons, they are combined into a Lisfranc joint, in which it is convenient to isolate part of the foot.
Intermetatarsal joints are flat, inactive.
The metatarsophalangeal joints are similar to the metacarpophalangeal joints. In the joints, flexion and extension is possible, as well as slight abduction and adduction. Moreover, extension is performed in larger sizes than flexion. Interphalangeal joints are similar to similar joints of the hand.
The joints of the toes are much less mobile than the joints of the fingers, although the shape of the joints in both is generally similar. The difference between the thumbs is especially striking. The big toe performs mainly flexion and extension in a small amount. The ability for abduction and opposition in this finger is practically lost. However, in human fetuses, the joint of the big toe has, like in anthropoids, a saddle shape. Through exercises, it is possible to significantly increase the mobility of both the tarsal-metatarsal joint of the first toe and the joints of other toes.
The bones of the foot have much less mobility than the bones of the hand, as they are adapted to perform a supporting function. Ten bones of the foot: navicular, three cuneiform, cuboid, five metatarsal bones - are interconnected with the help of "tight" joints and serve as a solid foundation for the foot. According to the concept of G. Pisani, in anatomical and functional terms, the foot is divided into the heel and talus parts. The heel part, which includes the calcaneus, cuboid, IV and V metatarsal bones, performs a predominantly passive static function. The talus, represented by the talus, navicular, sphenoid, I, II, III metatarsal bones, has an active static function.
The bones of the foot, articulating with each other, form 5 longitudinal and 2 transverse (tarsal and metatarsal) arches. I - III longitudinal arches of the foot do not touch the support plane when the foot is loaded, therefore they are spring, IV, V - are adjacent to the support area, they are called support. The tarsal arch is located in the region of the tarsal bones, the metatarsal arch is in the region of the heads of the metatarsal bones. Moreover, in the metatarsal arch, the support planes touch the heads of only the first and fifth metatarsal bones. Due to the arched structure, the foot does not rest on the entire plantar surface, but has constant 3 points of support: the calcaneal tubercle in the back and the heads of the I and V metatarsal bones in front. All longitudinal arches of the foot begin on the calcaneus. And from here the lines of the arches are directed forward along the metatarsal bones. The longest and highest is the 2nd longitudinal arch, and the lowest and shortest is the 5th. At the level of the highest points of the longitudinal arches, a transverse arch is formed.
The arches of the foot are held by the shape of the bones that form them, by ligaments (passive tightening of the arches of the top) and by muscles (active tightening). To strengthen the longitudinal arches, the long plantar ligament, the plantar calcaneonavicular ligament, and the plantar aponeurosis are of great importance as passive puffs. The transverse arch of the foot is held by transversely located ligaments of the sole (deep transverse metatarsal ligament, interosseous metatarsal ligaments). The muscles also help hold the arches of the foot. Longitudinally located muscles and their tendons, attached to the phalanges of the fingers, shorten the foot and thereby contribute to the "tightening" of its longitudinal arches, and the transversely lying muscles, narrowing the foot, strengthen its transverse arch. With the relaxation of active and passive puffs, the arches of the foot fall, the foot flattens, develops.