Epithelium in a smear - what does it mean? Epithelium in a smear: the norm in women. What does squamous epithelium in a smear mean in large quantities? Cytological smear: what is it
Epithelial tissue, or epithelium, covers the outside of the body, lines the cavities of the body and internal organs, and also forms most of the glands.
Varieties of the epithelium have significant variations in the structure, which depends on the origin (epithelial tissue develops from all three germ layers) of the epithelium and its functions.
However, all species have common features that characterize the epithelial tissue:
- The epithelium is a layer of cells, due to which it can protect the underlying tissues from external influences and exchange between the external and internal environment; violation of the integrity of the formation leads to a weakening of its protective properties, to the possibility of infection.
- It is located on the connective tissue (basement membrane), from which nutrients come to it.
- Epithelial cells have polarity, i.e. parts of the cell (basal) lying closer to the basement membrane have one structure, and the opposite part of the cell (apical) has another; each part contains different components of the cell.
- It has a high ability to regenerate (recovery). Epithelial tissue does not contain intercellular substance or contains very little of it.
Formation of epithelial tissue
Epithelial tissue is built from epithelial cells, which are tightly connected to each other and form a continuous layer.
Epithelial cells are always found on the basement membrane. It delimits them from the loose connective tissue, which lies below, performing a barrier function, and prevents the germination of the epithelium.
The basement membrane plays an important role in the trophism of epithelial tissue. Since the epithelium is devoid of blood vessels, it receives nutrition through the basement membrane from the vessels of the connective tissue.
Origin Classification
Depending on the origin, the epithelium is divided into six types, each of which occupies a specific place in the body.
- Cutaneous - develops from the ectoderm, localized in the oral cavity, esophagus, cornea, and so on.
- Intestinal - develops from the endoderm, lines the stomach of the small and large intestine
- Coelomic - develops from the ventral mesoderm, forms serous membranes.
- Ependymoglial - develops from the neural tube, lines the cavities of the brain.
- Angiodermal - develops from the mesenchyme (also called endothelium), lines the blood and lymphatic vessels.
- Renal - develops from the intermediate mesoderm, occurs in the renal tubules.
Features of the structure of epithelial tissue
According to the shape and function of cells, the epithelium is divided into flat, cubic, cylindrical (prismatic), ciliated (ciliated), as well as single-layer, consisting of one layer of cells, and multilayer, consisting of several layers.

| Table of functions and properties of epithelial tissue | |||
|---|---|---|---|
| Type of epithelium | Subtype | Location | Functions |
| Single layer epithelium | Flat | Blood vessels | BAS secretion, pinocytosis |
| Cubic | Bronchioles | Secretory, transport | |
| Cylindrical | Gastrointestinal tract | Protective, adsorption of substances | |
| Single layer multi-row | Columnar | vas deferens, duct of the epididymis | Protective |
| Pseudo stratified ciliated | Respiratory tract | Secretory, transport | |
| multilayer | transitional | Ureter, urinary bladder | Protective |
| Flat nonkeratinized | Oral cavity, esophagus | Protective | |
| Flat keratinizing | Skin | Protective | |
| Cylindrical | Conjunctiva | Secretory | |
| Cubic | sweat glands | Protective | |
single layer
Single layer flat The epithelium is formed by a thin layer of cells with uneven edges, the surface of which is covered with microvilli. There are single-nucleated cells, as well as with two or three nuclei.
Single layer cubic consists of cells with the same height and width, characteristic of the glands that excrete the duct. Single-layered cylindrical epithelium is divided into three types:
- Fringed - found in the intestines, gallbladder, has adsorbing abilities.
- Ciliated - characteristic of the oviducts, in the cells of which there are mobile cilia at the apical pole (contribute to the movement of the egg).
- Glandular - localized in the stomach, produces a mucous secret.
Single layer multi-row The epithelium lines the respiratory tract and contains three types of cells: ciliated, intercalated, goblet and endocrine. Together they ensure the normal functioning of the respiratory system, protect against the ingress of foreign particles (for example, the movement of cilia and mucous secretions help remove dust from the respiratory tract). Endocrine cells produce hormones for local regulation.
multilayer
Stratified squamous nonkeratinized the epithelium is located in the cornea, anal rectum, etc. There are three layers:
- The basal layer is formed by cells in the form of a cylinder, they divide in a mitotic way, some of the cells belong to the stem;
- spinous layer - cells have processes that penetrate between the apical ends of the cells of the basal layer;
- a layer of flat cells - are outside, constantly die off and exfoliate.
 Stratified epithelium
Stratified epithelium Stratified squamous keratinizing epithelium covers the surface of the skin. There are five different layers:
- Basal - formed by poorly differentiated stem cells, together with pigmented - melanocytes.
- The spinous layer together with the basal layer form the growth zone of the epidermis.
- The granular layer is built of flat cells, in the cytoplasm of which is the protein keratoglian.
- The shiny layer got its name because of its characteristic appearance during microscopic examination of histological preparations. It is a homogeneous shiny band, which stands out due to the presence of elaidin in the flat cells.
- The stratum corneum consists of horny scales filled with keratin. Scales that are closer to the surface are susceptible to the action of lysosomal enzymes and lose contact with the underlying cells, so they are constantly peeled off.
transitional epithelium located in the kidney tissue, urinary canal, bladder. Has three layers:
- Basal - consists of cells with intense color;
- intermediate - with cells of various shapes;
- integumentary - has large cells with two or three nuclei.
It is common for transitional epithelium to change shape depending on the state of the organ wall; they can flatten or acquire a pear-shaped shape.
Special types of epithelium
Acetowhite - this is an abnormal epithelium that becomes intensely white when exposed to acetic acid. Its appearance during a colposcopic examination makes it possible to identify the pathological process in the early stages.
Buccal - collected from the inner surface of the cheek, is used for genetic testing and establishing family ties.
Functions of epithelial tissue
Located on the surface of the body and organs, the epithelium is a border tissue. This position determines its protective function: protection of the underlying tissues from harmful mechanical, chemical and other influences. In addition, metabolic processes occur through the epithelium - the absorption or release of various substances.
The epithelium, which is part of the glands, has the ability to form special substances - secrets, as well as release them into the blood and lymph or into the ducts of the glands. Such an epithelium is called secretory, or glandular.
Differences between loose fibrous connective tissue and epithelial
Epithelial and connective tissue perform various functions: protective and secretory in the epithelium, supporting and transport in the connective tissue.
The cells of the epithelial tissue are tightly interconnected, there is practically no intercellular fluid. The connective tissue contains a large amount of intercellular substance, the cells are not tightly connected to each other.
When visiting a gynecologist, it is always necessary to take a smear on the flora. With it, you can determine the condition of the vaginal mucosa and the presence of infections. Only a doctor who knows the norms of all indicators can correctly decipher the smear. The epithelium in the smear may indicate the presence of an inflammatory process, which may be associated with various causes.
Indications for the purpose of the analysis
There are certain reasons that require a vaginal or urethral swab test to determine the presence of infections or inflammation in the reproductive system:
- pain localized in the lower abdomen;
- taking antibiotics for a long time;
- the presence of suspicious discharge from the vagina, bringing discomfort;
- sensation of itching and burning in the genital area;
- pregnancy planning;
- carrying out a preventive examination.
If you have unpleasant symptoms, you should immediately visit a doctor and take a smear and analysis for the presence of genital infections. What epithelium means in a smear depends on the characteristics of its cells and their structure and quantity.
Rules for preparing for analysis
To get a reliable result, you must:
- two days before the smear, exclude sexual intercourse;
- do not use vaginal contraceptives (including condoms, ointments, lubricants and creams) and suppositories;
- stop douching two days before the test;
- do not conduct examinations during menstruation, since menstrual blood significantly distorts the results of the analysis, and can show that the epithelium in the smear is increased, the most correct option would be to take a smear in the first days after the end of menstruation;
- you should not use means for intimate hygiene the day before, it is necessary to carry out hygiene procedures of the genital organs simply with warm water without using any detergents;
- you can not go to the toilet two hours before the test.

Proper preparation for the smear will allow you to most accurately determine the number of cells in it and assess the health of the reproductive system. The epithelium in the smear indicates the condition of the mucous membrane of the vagina and cervix. When the norm changes, it can be concluded that there is inflammation or atrophy of the epithelial layer.
Swab technique
A smear for cytology is taken using a special spatula, which is available in a standard gynecological examination kit. It is necessary to take an analysis at the place of transformation (where the squamous epithelium turns into a cylindrical one), after taking the material is distributed over a glass slide.
The transformation zone is located in the area of the external os, but in some cases (depending on the hormonal balance and age) it can change its position. Taking a smear from the transitional epithelium is necessary to accurately determine the presence of malignant cells. Since they appear from the lower layers, taking a smear from the location of the surface epithelium, it will be possible to diagnose cancer only at the last stage.

That is why the epithelium in the smear plays a very important role. The norm in women ranges from 3-15 units in the field of view. If their number is higher, additional examinations should be carried out to detect a malignant tumor.
What is squamous epithelium and its significance in a smear
The squamous epithelium is the lining of the vagina. Depending on the phase of the menstrual cycle, the cells may undergo minor changes. The surface epithelium is divided into keratinized and non-keratinized, the ratio of cells changes in different phases, so this fact must be taken into account in order to determine whether the obtained indicators are the norm.
The epithelium in a smear is normal only if its number does not exceed 15 units in the field of view. Exceeding the norm indicates the presence of inflammation, or a recent infection. When the structure of cells changes, suspicions arise for the development of a benign or malignant tumor.
The value of the cylindrical epithelium in the smear
The epithelium in the smear, which has a cylindrical shape, is functional, as it provides the secretion of mucus on the cervix. Normally, columnar epithelium in a smear is represented by cell groups that have a honeycomb-like or linear structure.
In addition, goblet-shaped cells can be found, their difference is in the cytoplasm stretched with mucus. In some cases, these cells may contain secretion granules. A common pathology - ectopia, is a shift in the location of the cylindrical epithelium and its replacement with a flat surface epithelium.
Further diagnostic measures
If an epithelium was found in a smear, the norm of which is violated, the doctor can make a diagnosis - vaginitis. In addition to a high concentration in the analysis of epithelial cells, a woman should have an uncomfortable discharge that has an unpleasant odor, itching and pain are felt in the vagina, and redness of the vulva is also observed.

Treatment of vaginitis is carried out with the help of antibiotics, which are combined with the use of antifungal or other drugs, depending on the type of pathogen.
Treatment of non-infectious vaginitis
If the epithelium in the smear on the flora is increased, and no infections were found, it can be concluded that there is a non-infectious pathogen. These can be hygiene products containing chemicals that cause irritation of the mucous membrane, contraceptives, with increased sensitivity of the vagina to spermicides.
In these cases, it is enough to stop using the funds, and after a while the concentration of the epithelium in the smear itself will recover to normal levels. To accelerate the effect, you can use suppositories or tablets that normalize the microflora of the vagina and allow normal cells to recover faster.
Epithelium in a smear in men
A high content of epithelial cells in a smear can be observed not only in women, but also in men. The most common disease, accompanied by an increased amount of epithelium, is urethritis. In men, urethritis is accompanied by pain and burning when urinating, discomfort and swelling in the genital area and groin, discharge from the penis or blood in the urine and semen.

Female urethritis is accompanied by chills, pain in the lower abdomen, frequent urge to urinate, burning and pain, as well as the presence of atypical vaginal discharge.
The causative agents of urethritis can be:
- cytomegalovirus;
- herpes simplex virus;
- chlamydia;
- gonococci.
If any virus or bacteria is detected, additional examinations and the appointment of effective treatment are required.
Atypical epithelial cells in a smear
In some cases, atypical epithelium may be detected in a smear. What does it mean? Altered structure of the cells of the squamous epithelium lining the vagina and cervix may indicate the development of cancerous tumors or dysplasia.
Cervical dysplasia causes cancer in only one percent of women. In other cases, with regular monitoring and treatment, it disappears after a few years. If the disease continues to develop and there is a risk of developing cancer cells, the doctor may advise a hyperectomy - removal of the uterus and cervix.

Most often, this procedure is performed for women with menopause or women who no longer plan to give birth.
Methods for eliminating atypical cells
In the presence of a large amount of atypical epithelium, radical methods may be required to destroy the cells. After that, the number of cells is normalized, and the epithelium in the smear is restored. The norm in women during the recovery period is individual, therefore, after surgical interventions, after a while, you need to visit a gynecologist and again take a smear test.
For the treatment of dysplasia, as a rule, the following methods are used:
- Laser therapy is the most modern and effective way. In addition to removing the atypical area, you can also explore its depth and act on all layers of the tissue. This procedure is very painful and traumatic, so bleeding may begin after a few days.
- Diathermy - cauterization, is the effect of electricity on an atypical area. It is the fastest and easiest method. After cauterization, scars may remain on the cervix, which in some cases cause infertility.
- Cryothermy - exposure to the damaged area with ultra-low temperatures. The method is effective only in the initial stages of dysplasia. With the development of cancer cells or the occurrence of atypical processes in the cells of the basal layer, it does not bring any results.
All these procedures are aimed at the destruction of atypical cells under the influence of temperature or a laser beam. In place of the destroyed cells, cells of squamous and cylindrical epithelium appear, which are the norm for the cervix and vagina.

The epithelium in the smear, the norm of which has been restored after such procedures, will not carry the risk of developing cancer. If the treatment procedures have not been effective, it is highly likely that a hyperectomy (removal of the uterus and cervix) will have to be performed.
The mucous membranes of the female genitourinary system are composed of squamous epithelium. Cylindrical epithelium is also found, it lines the cervical canal. Its cells secrete a certain secret and help protect the mucous membrane of the organ from external damage. Cylindrical epithelium in a smear below or above normal may indicate a malfunction in the hormonal background of a woman or the presence of inflammation.
The function of the columnar epithelium is to provide the necessary amount for its lubrication. In the normal state, the cells of such an epithelium are dispersed over the surface of the cervical canal in groups that are shaped like honeycombs, strips or glasses. The latter depends on the prolongation of the cytoplasm with mucus.
Deviations from the norm and consequences:
- the displacement of the cylindrical epithelium and the replacement of squamous cells by it speaks;
- a low number of cylindrical epithelium cells indicates hormonal imbalance;
- a lot of atypical cylindrical epithelium is the development of cancerous pathologies in the cervix;
- an increase in atypical cylindrical cells may indicate infectious diseases of the genitourinary system of a woman, in particular the urethra, the presence of inflammatory processes (, erosion);
- post-traumatic disorders - the formation of fistulas in the vagina and cervix,.
- the absence of a cylindrical epithelium in a smear may indicate the death of its cells, which is a prerequisite for the development of cervical dysplasia.
Important! Intensive growth of atypical cells, both cylindrical and may indicate the development of benign mastopathy. Negative pathological processes in the mammary glands of a woman can provoke changes in the mucous membranes of the organs of the genitourinary system.
Factors affecting the number of cells in the mucous layer of the reproductive organs

Basically, all organs in the human body are lined with squamous epithelial cells. Among them, there is also a cylindrical epithelium, which is mostly located in the cervical canal. Its main function is secretory. The presence of such a layer is responsible for the formation of a barrier to the negative effects of the external environment.
Reasons for changing the amount of columnar epithelium in a woman's smear:
- The presence of infections in the genitals that cause inflammation. This may be the entry into the body of gardnerella, streptococci, chlamydia. Also, the formation of atypical cells of the cylindrical epithelium can be affected by the human papillomavirus.
- Traumatism of the cervix as a result of difficult childbirth, curettage during abortion and other disorders of the epithelial layer.
- Hormonal disruptions are provoked by an increase in the level of estrogen in the blood. At this time, the replacement of squamous epithelium with a cylindrical one is provoked by the occurrence of such diseases as: papillomas, endometriosis, fibroma, ovarian dysfunction, and menstrual cycle disorders.
- Weakened immune system of a woman.
- Early onset of sexual activity. Pathological growth of cylindrical cells can be provoked by early sexual acts, during which the epithelial layer that has not yet been formed could be damaged.
- Active sex life, which is accompanied by a constant change of sexual partners.
Note! Pathological changes in the cylindrical epithelium are almost always accompanied by some signs. Their presence should encourage women to turn to a specialist.
Symptoms of the development of pathological changes in the mucous membranes
An increase in the amount of cylindrical epithelium, in the flesh, until it replaces squamous cells, in a neglected form causes a certain discomfort in the genitourinary system, which a woman cannot help but notice. Any more negative manifestations indicate the presence of pathological changes in the reproductive organs.
The main symptoms of changes in the cylindrical epithelium:

- The presence of copious discharge with the appearance of an odor, which is accompanied by itching or burning.
- The appearance of pain during intimate relationships, as well as the presence of blood whites after.
- Violations in the cycle of menstruation, which provoke long-term infertility.
Important! In the early stages, slight deviations in the smear do not have obvious signs. That is, in this case, the doctor can detect any violations only at the next gynecological examination by taking a smear on the flora.
Diagnosis of the disease and methods of treatment
Identification of a disease of the genitourinary system begins with a gynecological examination and taking a smear. Such an analysis allows you to identify the presence and quantity of both squamous and cylindrical epithelium, detect leukocytes that indicate inflammatory processes and prescribe a further clarifying examination.
Normally, the cylindrical epithelium in a woman's smear should be no more than 4–15 cells that fall into the field of view. Exceeding the norm indicates the presence of pathology in the cervical canal and uterus. If there are very few cells, then we are talking about hormonal disruptions. The complete absence of epithelial cells may indicate cervical dystrophy and be the cause of infertility.
Analysis by taking a smear from the uterus and its canal makes it possible to determine the presence of atypical cells in the mucous membranes of the reproductive organs. Their presence suggests that malignant pathologies develop in the cervical canal. A smear in which a large number of atypical cells of the cylindrical epithelium indicates a precancerous or cancerous condition.
If, after examining the smear, a significant replacement of the squamous epithelium with a cylindrical one was revealed, then the patient may be prescribed other methods of examination - cytological studies, bacterial cultures based on the smear, hormonal background, immunogram.
Squamous cell carcinoma- malignant neoplasm tumor), which develops from epithelial tissue ( epithelium) skin and mucous membranes. This disease is characterized by relatively rapid development and aggressive course. Starting in the skin or in the mucous membrane, the cancer process quickly affects the local lymph nodes and grows into neighboring organs and tissues, disrupting their structure and function. Ultimately, without appropriate treatment, multiple organ failure develops with a fatal outcome.
Squamous cell carcinoma accounts for approximately 25% of all types skin cancer and mucous membranes. In almost 75% of cases, this tumor is localized in the area of the skin of the face and head. The disease occurs more frequently in the elderly ( after 65 years), somewhat more common in men.
Interesting Facts
- Squamous cell skin cancer is more common in Caucasians.
- People who burn quickly in the sun are prone to developing squamous cell skin cancer.
- The most dangerous time for sunbathing is from 12.00 to 16.00, since in this period the ultraviolet radiation of the sun is maximum.
- Squamous cell carcinoma in children develops in extremely rare cases, in the presence of a genetic predisposition.
Causes of squamous cell carcinoma
 The exact causes of squamous cell carcinoma have not yet been established. An important role in the development of the malignant process is played by a decrease in the protective functions of the body and excessive exposure to various damaging factors.
The exact causes of squamous cell carcinoma have not yet been established. An important role in the development of the malignant process is played by a decrease in the protective functions of the body and excessive exposure to various damaging factors. squamous epithelium in humans
Epithelial tissue is a layer of cells covering the surface of the body, lining the organs and cavities of the body. Squamous epithelium is one of the varieties of epithelial tissue and covers the skin, as well as the mucous membranes of some internal organs.Depending on the structure, there are:
- Stratified squamous nonkeratinized epithelium. Composed of three layers of cells ( basal, spinous and superficial). Spiny and superficial layers are separate stages of maturation of the cells of the basal layer. The cells of the surface layer gradually die and exfoliate. This epithelium lines the cornea of the eye, the mucous membrane of the mouth and esophagus, the mucous membrane of the vagina and the vaginal part of the cervix.
- Stratified squamous keratinized epithelium ( epidermis). Lines the skin and is represented by four layers of cells ( basal, spiny, granular, horny). In the area of the palms and soles there is also a fifth layer - shiny, located under the stratum corneum. Epidermal cells are formed in the basal layer, and as you move to the surface ( horny) layer they accumulate protein keratin, they lose their cellular structure and die. The stratum corneum is represented by completely dead cells ( horny scales), filled with keratin and air bubbles. Horny scales are constantly peeling off.
Risk factors in the development of squamous cell carcinoma
There are a number of predisposing factors ( carcinogens), the impact of which on the skin, mucous membranes and on the body as a whole can contribute to the development of a malignant process.Factors contributing to the occurrence of cancer are:
- genetic predisposition;
- ultraviolet radiation;
- taking immunosuppressants;
- ionizing radiation;
- tobacco smoking;
- malnutrition;
- alcoholic drinks;
- professional hazards;
- contaminated air;
- age.
Modern research in the field of genetics and molecular biology allows us to state with confidence that the predisposition to the development of squamous cell carcinoma can be determined at the gene level.
Genetic predisposition is expressed through:
- Violations of the antitumor defense of the cell. Each cell of the body has a specific gene responsible for blocking the development of malignant tumors ( the so-called anti-oncogene, "guardian of the genome"). If the genetic apparatus of a cell ( providing cell division) is not disturbed, this gene is in an inactive state. When DNA is damaged deoxyribonucleic acid responsible for the storage, transmission and reproduction of genetic information) this gene is activated and stops the process of cell division, thus preventing the formation of a tumor. When a mutation occurs in the anti-oncogene itself ( occurs in more than half of all squamous cell carcinomas) its regulatory function is impaired, which may contribute to the development of the tumor process.
- Violations of the functioning of antitumor immunity. Every minute, thousands of gene mutations occur in the human body, that is, potentially thousands of new tumors are formed. However, thanks to the immune system ( so-called antitumor immunity), tumors do not develop. Several types of cells are involved in providing antitumor immunity ( T-lymphocytes, B-lymphocytes, macrophages, natural killer cells), which very quickly recognize and destroy mutant cells. With mutations in the genes responsible for the formation and functioning of these cells, the effectiveness of antitumor immunity may decrease, which creates favorable conditions for the occurrence of malignant neoplasms. Gene mutations can be passed from generation to generation, causing a predisposition to tumor processes in offspring.
- Impaired metabolism of carcinogens. When any carcinogens enter the body ( physical or chemical) certain protective systems are activated, aimed at neutralizing them and removing them as soon as possible. When the genes responsible for the operation of these systems are mutated, the risk of developing a tumor process increases.
Ultraviolet rays are the part of solar radiation that is invisible to the naked eye. The impact of these rays on human skin ( with prolonged exposure to the sun or with frequent use of the so-called ultraviolet baths for artificial tanning) causes various genetic mutations, which leads to the emergence of potential tumor cells, and also weakens the antitumor defense of the cell ( due to mutations in an anti-oncogene).
With prolonged and intense exposure to ultraviolet rays, antitumor immunity may not be able to neutralize all cells with a mutant genome, which will lead to the development of squamous cell skin cancer.
Taking immunosuppressants
Some medicines ( azathioprine, mercaptopurine and so on), used in various diseases and pathological conditions ( tumors of the blood system, autoimmune diseases, organ transplants) have a depressing effect on the body's defense systems, including antitumor immunity. The use of such drugs can lead to the development of squamous cell carcinoma.
ionizing radiation
Ionizing radiation includes x-rays, gamma rays, hydrogen and helium nuclei. Influencing the body, ionizing radiation has a damaging effect on the genetic apparatus of cells, leading to the emergence of numerous mutations. In addition, damage to the body's immune system leads to a weakening of antitumor immunity, which increases the likelihood of developing cancer hundreds of times.
Many epidemiological studies have shown that squamous cell carcinoma and other forms of malignant neoplasms occur hundreds of times more often in individuals exposed to these types of radiation ( with frequent use of ionizing radiation for medical purposes, among workers in the nuclear industry, in case of accidents at nuclear power plants and explosions of atomic bombs).
Tobacco smoking
It has been scientifically proven that smoking cigarettes and other products containing tobacco ( cigars, pipes) increases the risk of developing squamous cell carcinoma of the oral cavity, organs of the digestive system and respiratory tract. At the same time, both active smokers are susceptible to carcinogenic action ( direct smokers) and passive ( surrounding, inhaling tobacco smoke).
The combustion of tobacco during puffing occurs at very high temperatures, as a result of which, in addition to nicotine, many other combustion products enter the body ( benzene, formaldehyde, phenols, cadmium, chromium and others), the carcinogenic effect of which is scientifically proven. When a cigarette is smoldering not during tightening) the combustion temperature of tobacco is lower, and much less carcinogens are released into the environment.
Carcinogenic substances, absorbed through the mucous membranes of the oral cavity and respiratory tract, have a local carcinogenic effect. In addition, being absorbed into the blood and spread throughout the body, they can cause the development of tumors in various organs and tissues.
In many countries, tobacco is used for more than just smoking ( there is snuff, chewing tobacco). These methods of use do not ingest the substances formed during the combustion process, however, other carcinogens are released that increase the risk of developing cancer of the lips, mouth and pharynx.
Improper nutrition
Proper, balanced nutrition ensures the normal development and functioning of the body's immune system, in particular, antitumor immunity, which reduces the likelihood of developing cancer.
It has been scientifically proven that excessive consumption of animal fats in the diet significantly increases the risk of developing cancer of the digestive system. At the same time, plant foods vegetables and fruits) contain vitamins ( A, C, E, folic acid) and other substances ( selenium) to prevent tumor growth. Their lack in the diet can significantly increase the risk of developing malignant neoplasms.
Alcoholic drinks
Directly ethyl alcohol ( active ingredient in all alcoholic beverages) does not cause the development of malignant neoplasms. At the same time, the relationship between alcohol abuse and the risk of developing cancer has been scientifically proven. This is because alcohol increases the permeability of cells to various chemicals ( benzapyrene and other carcinogens). This fact is confirmed by the most frequent localization of squamous cell carcinoma in alcoholics in the oral cavity, larynx and pharynx, that is, in organs that are in direct contact with ethyl alcohol and its vapors.
The likelihood of developing squamous cell carcinoma in these areas is several times higher when alcohol is combined with smoking or another method of using tobacco.
Occupational hazards
Inhalation of certain chemicals, as well as intense and prolonged exposure to the skin, can lead to the development of squamous cell carcinoma. A more important role is played by the duration of exposure to carcinogens than their concentration.
Occupational carcinogens in people of various professions
Contaminated air
It has been proven that the risk of developing respiratory tract cancer is significantly higher in people living near industrial enterprises ( metallurgical, oil refineries). Also, the population of large cities is more susceptible to the risk of developing cancer. The abundance of transport in megacities causes the release into the air of a large amount of exhaust gases containing soot, which is a carcinogen.
infections
It has been scientifically proven that certain viruses can contribute to squamous cell carcinoma.
The occurrence of squamous cell carcinoma may be due to:
- Human papillomavirus. This virus can cause the development of various benign tumors in the skin and mucous membranes ( warts, papillomas), and in very rare cases can cause cervical cancer. Introducing itself into the DNA of body cells, the virus changes their structure, which leads to the formation of new copies of the virus in the cell. This process can lead to the emergence of various mutations at the genome level, up to the onset of a malignant process.
- Human Immunodeficiency Virus (Human Immunodeficiency Virus) HIV). This virus infects the cells of the immune system, which ultimately leads to the development of human acquired immunodeficiency syndrome ( AIDS), which reduces both anti-infective and anti-tumor defenses of the body.
Squamous cell carcinoma, in the vast majority of cases, occurs in people over 65 years of age. This is due to the fact that in the process of aging there is a decrease and violation of the functions of almost all organs and systems of the body, including the immune system. The antitumor protection of the cell is disrupted, as well as the processes of recognition and destruction of mutant cells worsen, which significantly increases the risk of squamous cell carcinoma.
Precancerous diseases
Certain diseases of the skin and mucous membranes, while not being malignant, increase the risk of developing squamous cell carcinoma.Depending on the likelihood of developing cancer, there are:
- obligate precancerous diseases;
- facultative precancerous diseases.
This group of precancers includes a number of skin diseases which, without appropriate treatment, always degenerate into a cancerous tumor.
Obligate precancers are:
- Pigmented xeroderma. A rare hereditary disease transmitted in an autosomal recessive manner ( a child will only get sick if they inherit the defective gene from both parents). Appears in children aged 2-3 years and is externally manifested by redness of the skin, the formation of cracks, ulcerations, warty growths in open areas of the body. The mechanism of development of this disease is explained by a violation of the resistance of cells to the action of ultraviolet rays. As a result, when sunlight hits the skin, DNA damage occurs. With each new exposure to a damaging factor, the number of mutations in cells increases, which ultimately leads to the development of cancer.
- Bowen's disease. A rare skin disease that occurs as a result of prolonged exposure to adverse factors ( chronic trauma, prolonged exposure to the sun, occupational hazards). It is externally manifested by one or more small red spots, located mainly on the skin of the body. Over time, a red-brown plaque forms in the affected area, from the surface of which scales are easily separated. With the development of squamous cell carcinoma, the surface of the plaque ulcerates.
- Paget's disease. A precancerous disease that mainly affects women. Characterized by the appearance on the skin ( in the vulva and in the axillary region) redness, which has clear boundaries. The surface may be wet or dry, flaky. The affected area can increase over several years, degenerating into squamous cell carcinoma.
This group includes diseases, the presence of which will not necessarily lead to the occurrence of squamous cell carcinoma, but the likelihood of its development in this case is increased several times.
Optional precancers are:
- Senile keratosis. It occurs in older people, mainly in areas of the skin that are not covered by clothing. The main reason is considered to be prolonged exposure to ultraviolet rays. As a result, reddish plaques appear on the skin of the hands and on the face, ranging in size from a few millimeters to a centimeter. Their surface is covered with hard, yellowish scales, which are difficult to separate from the skin. The probability of developing squamous cell carcinoma in this disease reaches 25%.
- Skin horn. It is hyperkeratosis pathological thickening of the stratum corneum of the epidermis), manifested by local deposition of horny masses ( scales). As a result, a cylindrical or cone-shaped horn protruding above the skin is formed, the length of which can reach several centimeters. The development of cancer is observed in 7 - 15% of cases and is characterized by the germination of the formation deep into the skin.
- Keratoacanthoma. A disease that occurs predominantly in people over 60 years of age. It is a formation of a round shape up to several centimeters in diameter, in the center of which there is a depression filled with horny masses ( scales of yellow). It is located on the skin of the face or the back of the hands.
- contact dermatitis. It develops as a result of exposure to the skin of various chemicals, cosmetic creams. It is characterized by a local inflammatory reaction, redness and swelling of the affected area, itching and burning sensation may appear. With the long-term existence of this process, various disorders occur in the cellular structure of the skin, which ultimately can lead to the development of cancer.
The mechanism of development of squamous cell carcinoma
 As a result of exposure to risk factors, a gene mutation occurs in one of the cells of the spinous layer of the stratified squamous epithelium, which is not eliminated by protective antitumor mechanisms. A mutated cell has a number of features that distinguish it from normal cells of the body.
As a result of exposure to risk factors, a gene mutation occurs in one of the cells of the spinous layer of the stratified squamous epithelium, which is not eliminated by protective antitumor mechanisms. A mutated cell has a number of features that distinguish it from normal cells of the body. A cancer cell is characterized by:
- Autonomy. Reproduction ( division) of normal body cells is regulated by the nervous and endocrine systems, as well as the number of cells themselves ( the more there are, the less they share). Tumor cells are deprived of any contact with regulatory mechanisms, resulting in their uncontrolled division.
- Immortality. Normal body cells can divide only a certain number of times, after which they die. The number of possible divisions is genetically determined and varies in different organs and tissues. In tumor cells, this process is disrupted, as a result of which an unlimited number of divisions is possible with the formation of many clones, which are also immortal and can divide an unlimited number of times.
- Self-sufficiency. During tumor growth upon reaching dimensions of 2 - 4 mm), tumor cells begin to produce special substances that stimulate the formation of new blood vessels. This process ensures the delivery of oxygen and nutrients to the deeper tumor cells, as a result of which the tumor can grow to a considerable size.
- Disruption of differentiation. In the process of development of epithelial cells, they lose the nucleus and other cellular elements, die and are rejected ( in stratified squamous nonkeratinized epithelium) or accumulate keratin and form horny scales ( in keratinized stratified squamous epithelium). In cancer cells, the differentiation process can be disrupted.
Depending on the degree of differentiation, there are:
- undifferentiated squamous cell carcinoma ( non-keratinizing). It is the most malignant form, characterized by rapid growth. In this case, the mutation occurs in the cell of the spinous layer, after which its development stops, and all subsequent clones have a similar structure. Keratin does not accumulate in cancer cells and the process of their death does not occur.
- Differentiated squamous cell carcinoma ( keratinizing). In this case, the mutation also occurs at the level of the spinous layer cell, however, after several divisions, the formed clones begin to accumulate a large amount of keratin. Cancer cells gradually lose their cellular elements and die, which is externally manifested by the deposition of crusts on the surface of the tumor ( keratin masses) yellowish. Unlike normal keratinization, with keratinizing cancer this process is accelerated several times.
Metastasis
This term refers to the process that results in the separation of tumor cell clones from the place of formation and their migration to other organs and tissues. Thus, secondary foci of tumor growth can form ( metastases). Cell division in secondary foci follows the same laws as in the primary tumor.Squamous cell carcinoma can metastasize:
- by the lymphatic route. This type of metastasis occurs in 98% of cases of squamous cell carcinoma. Through the lymphatic vessels, cancer cells can travel to the local lymph nodes, where they linger and begin to divide.
- By hematogenous way. Occurs only in 2% of cases. Tumor cells enter the blood vessels when their walls are destroyed, and with the blood flow they can migrate to almost any organ ( more often in the lungs, bones).
- by implantation. In this case, the spread of the tumor occurs through direct contact with neighboring organs, as a result of which tumor cells grow into the tissue of the organ, and the development of a secondary tumor begins in it.
Types of squamous cell cancer
 As already mentioned, squamous cell carcinoma is formed from the cells of the spiny layer of the stratified squamous epithelium. This section will describe the most common types of squamous cell carcinoma, although theoretically this neoplasm can develop in any organ covered with epithelium. This is possible with prolonged exposure to various damaging factors on epithelial cells, as a result of which their degeneration may occur ( metaplasia) with the formation of squamous epithelium in those organs where it is not normally found.
As already mentioned, squamous cell carcinoma is formed from the cells of the spiny layer of the stratified squamous epithelium. This section will describe the most common types of squamous cell carcinoma, although theoretically this neoplasm can develop in any organ covered with epithelium. This is possible with prolonged exposure to various damaging factors on epithelial cells, as a result of which their degeneration may occur ( metaplasia) with the formation of squamous epithelium in those organs where it is not normally found. So, when smoking, the ciliated epithelium of the respiratory tract can be replaced by a stratified squamous epithelium, and in the future, squamous cell carcinoma can develop from these cells.
Depending on the nature of growth, squamous cell carcinoma can be:
- Exophytic ( tumor). At the beginning of the disease, a dense nodule of skin color is formed. Its surface may initially be covered with yellow horny masses. It rapidly increases in size greater in height than in diameter). The base of the tumor is wide, inactive ( the tumor simultaneously grows into the deep layers of the skin and subcutaneous adipose tissue). Education is clearly delimited from unaffected skin. Its surface is uneven, bumpy, may be covered with scales or warty growths. In the later stages of development, the surface of the tumor nodes can ulcerate and turn into an infiltrative-ulcerative form.
- Endophytic ( infiltrative-ulcerative). At the beginning of the disease, a small dense nodule in the skin can be determined, which soon ulcerates. Around it, child ( secondary) nodules that ulcerate and merge with each other, causing an increase in the affected area. Tumor growth is characterized by an increase in the diameter and depth of the ulcer.
- Mixed. It is characterized by the simultaneous growth of the tumor node and ulceration of the skin and mucous membranes around it.
- skin;
- red border of the lips;
- oral cavity;
- esophagus
- larynx;
- trachea and bronchi;
- cervix.
Squamous cell skin cancer
One of the most common skin neoplasms. May be keratinizing ( in 90% of cases), and non-keratinizing. It develops mainly in open areas of the body ( on the skin of the face, neck, back of the hands). Can develop both ulcerative necrotic and neoplastic forms of cancer.Local manifestations of squamous cell skin cancer are:
- soreness;
- swelling of adjacent tissues;
- burning;
- violation of sensitivity;
- redness of the skin around the affected area.
Squamous cell carcinoma of the red border of the lips
Cancer of the lower lip is much more common, but cancer of the upper lip is characterized by a more rapid and malignant course. In most cases ( in 95%) develops keratinizing squamous cell carcinoma. Men are affected 3 times more often than women.Much more common is the infiltrative-ulcerative form, characterized by rapid development and aggressive course. The tumor form develops more slowly and rarely metastasizes.
Squamous cell carcinoma of the oral cavity
It is characterized by the development of a malignant neoplasm from the epithelium of the mucous membrane of the inner surface of the lips, cheeks, gums and palate.Risk factor for oral cancer in addition to the main ones listed above) is the frequent use of hot drinks and dishes. This leads to pathological changes in the epithelium ( normally being a multi-layered non-keratinizing), as a result of which keratinization zones appear, which can degenerate into a cancerous process.
Squamous cell carcinoma occurs in 95% of cases. Both forms of growth are equally common and are characterized by rapid development, germination into neighboring tissues and metastasis.
Symptoms of oral cancer are:
- Pain. It appears in the later stages of development and is due to the pressure of a volumetric formation on neighboring tissues. Pain may radiate to the head, nose, ears ( depending on the location of the tumor).
- Increased salivation. The tumor creates a sensation of a foreign body in the oral cavity, which reflexively increases the activity of the salivary glands.
- Bad breath. Appears in the late stages of the disease and is due to necrosis ( local extinction) tumor tissue and infection ( in the area affected by cancer, the barrier functions of the mucous membrane are disrupted, which creates favorable conditions for the growth and development of infectious microorganisms).
- Violation of the processes of chewing and speech. These manifestations are characteristic of the later stages of the disease, when the cancerous process grows into the masticatory and other muscles of the face, destroying them.
Squamous cell carcinoma of the esophagus
Squamous cell carcinoma accounts for up to 95% of all malignant neoplasms of the esophagus. An additional risk factor is the abuse of hot drinks and spicy foods, as well as gastroesophageal reflux disease ( GERD), characterized by the reflux of acidic gastric juice into the esophagus.By the nature of growth, the tumor-like form of squamous cell carcinoma is more common. The tumor can reach a considerable size, up to the complete overlap of the lumen of the esophagus.
Signs of esophageal cancer are:
- swallowing disorder ( dysphagia). It occurs due to the growth of a tumor in the lumen of the esophagus, which disrupts the movement of food. At first, it is difficult to swallow solid, and after a few months liquid food and even water.
- Pain in the chest. They appear in the later stages of development, due to compression of nearby tissues and organs by the tumor.
- Spitting up food. Pieces of food can get stuck in the tumor area and burp up a few minutes after eating.
- Bad breath. It develops in case of tumor necrosis and infection.
- Bleeding. Occurs when a cancerous process destroys the blood vessels in the esophagus ( more often veins) are often repeated. Manifested by bloody vomiting and the presence of blood in the stool. This condition is life-threatening and requires urgent medical attention.
Squamous cell carcinoma of the larynx
It accounts for about 60% of all malignant neoplasms of this organ. Both forms of the disease are equally common, however, infiltrative-ulcerative cancer is characterized by faster development and transition to neighboring organs.Signs of laryngeal cancer may include:
- Difficulty breathing. As a result of tumor growth, the lumen of the larynx may partially overlap, making it difficult for air to pass through. Depending on the location of the tumor node and its size, it may be difficult to inhale, exhale, or both.
- Voice change. It occurs when the cancerous process spreads to the vocal cords and can be manifested by hoarseness of the voice, up to its complete loss ( aphonia).
- Pain when swallowing. They can appear with a large size of the tumor node, squeezing the pharynx and upper esophagus.
- Cough. It occurs reflexively, as a result of mechanical irritation of the walls of the larynx. As a rule, it is not eliminated by antitussive drugs.
- Hemoptysis. It can occur with the destruction of blood vessels and as a result of the collapse of the tumor.
- Sensation of a foreign body in the throat.
Squamous cell carcinoma of the trachea and bronchi
The development of squamous cell carcinoma in the respiratory tract is possible as a result of previous metaplasia of the epithelium of the trachea or bronchi ( replacement of ciliated epithelium with squamous). Smoking and air pollution with various chemicals can contribute to this process.Cancer process can develop as exophytic ( protruding into the airway), and endophytic ( spreading in the walls of the trachea, bronchi and growing into the tissue of the lung).
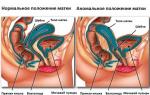
The mucous membrane of the vagina and the vaginal part of the cervix are covered with stratified squamous non-keratinized epithelium. Squamous cell carcinoma often develops in the area of transition of stratified squamous epithelium into cylindrical ( lining the internal os and uterine cavity).
Symptoms of a malignant neoplasm in the initial stages are nonspecific and may occur with other diseases of the genitourinary system.
Signs of cervical cancer may include:
- bleeding from the vagina outside of menstruation;
- bleeding after intercourse;
- constant aching pain in the lower abdomen;
- violation of urination and defecation.
What does squamous cell carcinoma look like?
The appearance of the tumor varies depending on the form of growth, the degree of differentiation and the affected organ.External characteristics of squamous cell carcinoma
| Type of cancer | growth shape | Description | Photo |
| Squamous cell skin cancer
| Infiltrative-ulcerative | It is a dense ulcerative defect of the skin, the edges of which are clearly delimited from intact areas. The surface is covered with a yellowish crust ( consisting of horny masses), upon removal of which an uneven, bleeding bottom of the ulcer is found. Nearby skin areas are inflamed ( red, swollen). |  |
| Tumor | A tumor-like formation rising above the skin on a wide base. On the surface, many small blood vessels are translucent. In the region of the apex, a small central depression of a dark brown color is determined, filled with yellowish horny masses, tightly adjacent to the tumor tissue. |  |
|
| Squamous cell carcinoma of the red border of the lips
| Infiltrative-ulcerative | It is an irregularly shaped ulcerative defect of the red border of the lips. The edges of the ulcer are clear, slightly undermined. The bottom is bumpy, covered with black areas of necrosis and yellow horny masses. |  |
| Tumor | A dense knot, rising on a wide base, which, without clear boundaries, passes to the mucous membrane of the lips and skin of the face. The surface is covered with horny crusts. In the center of the formation, a black necrosis focus is determined. The skin around it is deformed, inflamed, swollen. |  |
|
| Squamous cell carcinoma of the oral cavity | infiltrative | The affected mucous membrane is bright red, with a bumpy surface and jagged edges. In places, yellow crusts are determined, the removal of which causes bleeding. |  |
| Tumor | Nodular formation with clear, uneven edges. The surface is bumpy, rough, abundantly covered with horny masses. The surrounding mucous membrane is not changed. |  |
|
| Squamous cell carcinoma of the esophagus | Infiltrative-ulcerative | During endoscopic examination insertion of a flexible tube into the esophagus, at the end of which is a video camera) reveals an ulcerative defect of the mucous membrane of the esophagus, clearly delimited from intact tissue. The edges are raised, the surface is bumpy, slightly protruding into the lumen of the esophagus, it bleeds easily on contact. |  |
| Tumor | During endoscopic examination, multiple tumor formations of various sizes protruding into the lumen of the esophagus are determined. The base is wide, is a continuation of the mucous membrane. The surface is covered with many blood vessels. |  |
|
| Squamous cell carcinoma of the larynx | mixed | A volumetric formation of irregular shape is visually determined, with an uneven surface, on which yellow crusts and petechial hemorrhages are noted. The mucosa on the surface of the tumor and around it is ulcerated. |  |
| Squamous cell carcinoma of the trachea and bronchi | Tumor | During endoscopy, several tuberous cone-shaped outgrowths protruding into the lumen of the respiratory tract are determined. The surface is covered with a white coating, ulcerated, bleeding in places. |  |
| Squamous cell carcinoma of the cervix | Infiltrative-ulcerative | A gynecological examination reveals a reddened, ulcerated, bleeding cervix. The edges of the ulcer are clearly delimited and slightly raised above the mucous membrane. In some places yellow crusts are visible. |  |
| Tumor | It is characterized by the presence on the cervix of a volumetric formation on a wide base, protruding above the surface of the mucous membrane. Its surface is bumpy, rough, ulcerated and bleeding in places. |  |
Diagnosis of squamous cell carcinoma
 As a rule, pronounced clinical manifestations occur in the last stages of the disease, when there are multiple distant metastases. The prognosis in such cases is unfavorable. Timely and correct diagnosis of the cancerous process will allow the necessary treatment to be carried out in time, which can save a person's life.
As a rule, pronounced clinical manifestations occur in the last stages of the disease, when there are multiple distant metastases. The prognosis in such cases is unfavorable. Timely and correct diagnosis of the cancerous process will allow the necessary treatment to be carried out in time, which can save a person's life. The diagnostic process includes:
- examination by a doctor;
- instrumental research;
- laboratory research;
- tumor biopsy.
Examination by a doctor
A doctor of any specialty should be able to recognize a malignant neoplasm in the initial stages of its development. If squamous cell carcinoma of any localization is suspected, consultation with an oncologist is necessary.When should you see a doctor?
Some benign skin lesions ( papillomas and others) may go unnoticed for many years. However, there are certain external signs, the presence of which indicates a possible malignant degeneration of the neoplasm. It is important to recognize them in time and immediately consult a doctor, since in the case of the development of squamous cell carcinoma, treatment should be started as soon as possible.
Diagnostic criteria of the tumor process
| benign neoplasm | malignant neoplasm |
|
|
The doctor may ask clarifying questions:
- What is the patient's occupation?
- How long ago did the neoplasm appear?
- Does the neoplasm change over time ( in size or appearance)?
- Are there local symptoms pain, itching, or other symptoms)?
- What treatment was carried out and what are its results?
- Did family members and close relatives have similar neoplasms?
- general condition of the body;
- consistency and appearance of education;
- the color of the skin and mucous membranes directly around the neoplasm;
- nearby lymph nodes;
- the presence of similar formations in other parts of the body.
Instrumental research
They are used to establish a diagnosis and plan treatment tactics.For the diagnosis of squamous cell carcinoma are used:
- confocal laser scanning microscopy;
- thermography;
- endoscopic examination;
A modern high-precision method that allows you to get a layered image of the epidermis and upper layers of the skin. The advantage of this method is the ability to study suspicious neoplasms without prior sampling of material, directly on a person.
This method is absolutely harmless, does not require special training and can be used right at the doctor's office. The essence of the method is to place the area of the skin under examination under a special microscope, with which you can study all the layers of the epidermis, examine the structure of cells, their shape and composition. The method allows you to visually determine the presence of a tumor, the degree of differentiation and its germination in the deep layers of the skin.
thermography
A fairly simple, fast and safe method for detecting a malignant process. The essence of the method is to register the thermal radiation of the investigated area of the body. The patient takes off his outer clothing and sits in front of a special camera. To speed up the study, a small amount of water is applied to the surface of the skin with a sprayer.
Within a few minutes, the camera registers thermal radiation from normal and pathologically changed areas of the skin, after which it produces the so-called "thermal portrait" of the studied areas.
For squamous cell carcinoma, the definition of zones of elevated temperature is characteristic. This is due to the intensive growth of the tumor, as well as the presence of a large number of newly formed vessels.
Endoscopy
The essence of the method is the introduction of an endoscope ( a special tube with a camera at the end connected to a monitor) through natural routes or as a result of surgery. This study allows you to study the inner surface of the organ under study, visually determine the presence of a tumor, the form of its growth, the nature and degree of damage to the mucous membranes.
- Bronchoscopy- introduction of an endoscope into the respiratory tract and examination of the trachea and bronchi.
- Esophagoscopy- Examination of the inner surface of the esophagus.
- Laryngoscopy- examination of the vocal cords and mucous membrane of the larynx.
- Colposcopy- examination of the vagina and the vaginal part of the cervix.
The method is associated with certain risks ( bleeding, infection), in connection with which its implementation is possible only in specially equipped premises of a medical institution, in the presence of an experienced specialist.
Magnetic resonance imaging ( MRI)
A modern high-precision research method that allows you to get a layered image of various organs and tissues. The essence of the method is to create a strong electromagnetic field around the human body, as a result of which the nuclei of atoms begin to emit a certain energy, which is recorded by a tomograph and, after digital processing, is presented as an image on a monitor.
MRI allows:
- detect the presence of a tumor with a size of 5 mm;
- obtain information about the composition and shape of the tumor;
- determine the presence of metastases in various organs and tissues.
Laboratory research
If squamous cell carcinoma is suspected, additional laboratory tests may be ordered.Routine tests ( complete blood count, complete urinalysis) are not of particular diagnostic value in the detection of squamous cell carcinoma and are prescribed to determine the general condition of the body and identify possible concomitant diseases.
In the laboratory diagnosis of squamous cell carcinoma, the following is used:
- determination of tumor markers of squamous cell carcinoma;
- cytological study.
It is a specific laboratory test for diagnosing squamous cell carcinoma.
Tumor markers ( tumor markers) are substances of various structures produced by tumor cells. The specific marker for squamous cell carcinoma is the SCC antigen. It regulates the processes of differentiation ( maturation) of normal squamous epithelium, and also stimulates tumor growth in the case of squamous cell carcinoma.
An increase in the concentration of SCC antigen in the blood of more than 1.5 nanograms per milliliter may indicate in favor of squamous cell carcinoma of various localization. However, in some cases, the test may be false positive, and therefore the establishment of a final diagnosis only on the basis of the determination of this tumor marker is unacceptable.
An increase in the level of SCC antigen can be observed:
- with precancerous skin diseases;
- with other skin diseases ( eczema, psoriasis);
- with liver failure ( this antigen is destroyed in the liver, in case of violation of the functions of which its concentration may increase).
Cytological examination
The essence of the method is to study under a microscope the size, shape, structure and internal composition of tumor cells. A cytological preparation is subject to investigation ( smear) obtained in various ways.
The material for cytological examination may be:
- prints from the surface of the skin neoplasm;
- scrapings of the oral cavity, pharynx;
- biopsy smears ( biopsy material).
- Squamous cell carcinoma. It is characterized by the presence of large, irregularly shaped cells that lie scattered. The cell nucleus is enlarged, structurally changed, its color is more pronounced than in normal cells. Chromatin ( intranuclear genetic material of a living cell) is located unevenly. Cytoplasm ( internal environment of the cell) dense, there may be signs of early keratinization ( the presence of keratohyalin and keratin). Accumulations of horny scales can be determined between cells.
- Squamous cell nonkeratinizing cancer. Scattered cells or their clusters are determined. Their sizes and shapes are not the same. The cell nucleus is enlarged ( can occupy the whole cell) is located in the center. The chromatin in the nucleus is evenly distributed. Signs of keratinization are absent or slightly expressed.
Biopsy
It is the "gold standard" in the diagnosis of malignant neoplasms. The essence of the method lies in the intravital taking of a part of the suspicious material ( biopsy) from the surface of the skin or mucous membrane. The biopsy is subjected to special processing, after which it is examined under a microscope.Used to diagnose squamous cell carcinoma:
- incisional biopsy. After local anesthesia, a partial excision of the neoplasm fragment is performed. In this case, it is imperative to take both the tumor tissue and unchanged skin or mucous membrane.
- Needle biopsy. It is mainly used in the neoplastic form of squamous cell carcinoma. It is performed as follows - a special hollow needle with sharp edges is inserted deep into the tumor with rotational movements. As a result, all layers of the neoplasm fall into it, which makes it possible to further investigate their structure and relationship. The resulting material is transferred to a glass slide for further microscopic examination.
- Total biopsy. The entire tumor removed surgically is examined.
- external signs of a malignant neoplasm;
- questionable cytological data;
- the need to confirm the diagnosis of squamous cell carcinoma before starting treatment ( Necessarily).
 The essence of the method lies in the microscopic examination of the structure and cellular composition of the biopsy.
The essence of the method lies in the microscopic examination of the structure and cellular composition of the biopsy. The material obtained during the biopsy is fixed with 70% alcohol, after which it is sent to the laboratory for histological examination. In the laboratory, ultrathin sections of the preparation are carried out with a special knife, which are transferred to a glass slide, stained with special dyes and examined under a microscope.
Depending on the histological picture, there are:
- Keratinizing squamous cell carcinoma ( differentiated form). The structure of the tissue is broken, strands of tumor cells are determined, penetrating into the deep layers of the epidermis and skin. Cells are large, light, with large nuclei. In some of them, accumulations of keratin and keratohyalin are found ( signs of keratinization). Accumulations of keratin are determined between the strands ( horn pearls). In some places, processes of disturbed cell division are found ( mitosis).
- Non-keratinizing squamous cell carcinoma ( undifferentiated form). It is characterized by the presence of strands of tumor cells that disrupt the structure of the tissue. Tumor cells of various sizes, unequal shape ( round, oval, elongated) contain large nuclei. Very rarely, small pockets of keratinization can occur. The number of mitoses is many times greater than in the differentiated form.
Treatment of squamous cell cancer
 Treatment of squamous cell carcinoma is prescribed only by an oncologist and only after a complete and detailed examination, depending on the stage and form of the disease. Self-medication is unacceptable and is life-threatening.
Treatment of squamous cell carcinoma is prescribed only by an oncologist and only after a complete and detailed examination, depending on the stage and form of the disease. Self-medication is unacceptable and is life-threatening. Depending on the stage of cancer, there are:
- 0 stage - a small tumor located in the epidermis or in the superficial sections of the mucous membrane. There are no metastases.
- I stage - tumor up to 2 cm in greatest dimension, does not grow into underlying structures. There are no metastases.
- II stage - the tumor is more than 2 cm, but does not grow into the underlying tissues. There are no metastases.
- III stage - the tumor grows into the underlying tissues ( into the skin, muscles, into the walls of organs). Metastases to local lymph nodes.
- IV stage - There are distant metastases to other organs. The size of the tumor does not matter.
- surgery;
- drug treatment;
- other treatments;
- symptomatic treatment.
Radiation therapy
It is the method of choice in the treatment of stage I-II squamous cell carcinoma of any localization. The essence of the method lies in the high-precision impact of ionizing radiation on the tumor focus, which leads to disruption of the processes of division of cancer cells. Thanks to modern technology, the degree of radiation damage to healthy tissues is minimal.For stage III-IV tumors, radiation therapy is used in the preoperative period to slow down the growth and reduce the size of the tumor, after which it is surgically removed.
The duration of radiation therapy depends on the histological variant of the tumor. Highly differentiated squamous cell carcinoma requires longer treatment and higher doses of radiation than undifferentiated.
If a relapse occurs after radiotherapy ( development of squamous cell carcinoma in the same site), then repeated application of this method is inefficient.
Surgery
Surgical removal of the tumor is indicated for stages III-IV of squamous cell carcinoma in combination with radiation and chemotherapy ( drug treatment) or at stages I - II with the ineffectiveness of radiation therapy.The operation is performed under local or general anesthesia ( depending on the size and location of the neoplasm). The tumor is removed, capturing 2 centimeters of healthy, unchanged tissue from each of its edges. Both the tumor itself and the underlying structures into which it grows are removed ( muscles, bones, up to amputation of a limb or removal of an affected organ). If there are metastases in the local lymph nodes, they are also completely removed.
The removed material must be sent for histological examination.
Medical treatment
Rather, it is an alternative method, since the effectiveness of drug therapy for squamous cell carcinoma is variable. It is usually used in the preoperative period to reduce the size of the tumor or in combination with radiation therapy for the treatment of inoperable cancer and metastases.Chemotherapy for squamous cell carcinoma
| Name of medication | Mechanism of action | Dosage and administration |
| Bleomycin | Antitumor antibiotic. Destroys the DNA molecule at the beginning of cell division, also inhibiting cell growth. | It is administered intravenously, diluted in 20 ml of 0.9% sodium chloride solution. Inject slowly over 5 minutes. Dosage:
|
| Cisplatin | Antitumor agent. Violates the process of DNA synthesis, which leads to the death of the tumor cell. | It is administered intravenously, drip, slowly, diluted in 0.9% sodium chloride solution. The recommended dose is 2.5 mg per 1 kg of body weight, every 4 weeks. During treatment, it is necessary to regularly check the cellular composition of the blood. |
| 5-fluorouracil | An antitumor drug with a cytostatic effect. Selectively accumulating in cancer cells, it disrupts the process of DNA synthesis, which leads to a stop of cell division. | The solution is administered intravenously, drip or jet, at a dose of 12 mg per kilogram of body weight for 5 days. Break between courses 4 weeks. |
| Ointment for external use, used for squamous cell skin cancer. It is applied once a week on the surface of the tumor with a thin layer, not rubbed. The course of treatment is determined individually depending on the course of the disease. |
Other Treatments for Squamous Cell Cancer
These methods are used less frequently, as indications for them are limited. At the same time, with the right choice of method, a complete cure of the disease is possible.Alternative treatments are:
- Electrocoagulation. Used to remove small diameter up to 1 cm), superficially located tumors in the face, neck, lips. Healthy tissues are also removed within 5-6 mm from the tumor. The advantage of this method is low trauma, which is good in cosmetic terms.
- cryogenic treatment. It is used mainly for squamous cell skin cancer up to 1 cm in diameter, which does not grow into deep tissues. The essence of the method is to freeze the tumor and adjacent tissues with liquid nitrogen ( whose temperature is -196 ºС). The advantage of cryotherapy is a good cosmetic effect. The main disadvantage is the impossibility of histological examination of the removed material.
- Photodynamic therapy. The essence of the method is as follows. At the first stage, the surface of the tumor is treated with a special chemical ( e.g. hematoporphyrin), which has the ability to selectively accumulate in cancer cells. The second stage is a laser effect on the tumor area, as a result of which hematoporphyrin is activated and stimulates the formation of highly toxic compounds ( oxygen free radicals), which leads to the destruction of tumor cells. Healthy tissues are not damaged.
Symptomatic treatment
It is carried out in the presence of complications of the tumor itself or with the development of side effects of radiation and drug therapy.Squamous epithelium in a smear for flora and cytology defined in all women. Those who are of reproductive age and do not breastfeed have more than those who are lactating, in the absence or exhaustion of the ovaries, menopause (menopause) - in general, than those who do not have a menstrual cycle.
For reference: estrogens continue to be produced in menopausal women and with removed ovaries, as they are also produced by the adrenal glands.
The epithelium has a protective function. Thanks to him, the vaginal microflora remains rod-shaped, the environment is acidic, unacceptable for the reproduction of pathogens. The epithelial layer may decrease somewhat when taking hormonal contraceptives and glucocorticosteroids.
What types of smear are used to diagnose the presence of squamous epithelium? You can see these words in the results of a smear on the flora (the so-called total smear) and cytograms. In this case, the first will indicate only the amount of epithelium. But in the conclusion of a cytological study (Pap test) there is more information, in the description there will be qualitative characteristics.
Types of epithelial cells and dependence on estrogen
The squamous or stratified epithelium is the cells that line the vaginal part of the cervix. In the cervical canal, another type of epithelium is cylindrical. Flat consists of four types of cells - superficial, intermediate and basal-parabasal layer.
Which cells the doctor will take for analysis depends on the concentration of the main female hormone - estrogen. Flat epithelium in layers, fragments, clusters in a smear - these are all variants of the norm, if without anaplasia.
Superficial, the largest, but with a small nucleus, cells are characteristic of days 9-14 of the menstrual cycle. If, as a result of the analysis, it is written that there is a large amount of epithelium, and you passed it just in the middle of the cycle, then this is the reason.
Intermediate cells occur at any phase of the cycle. Their difference is a slightly smaller size, irregular shape, larger core size.
While estrogen is at its lowest point, during menstruation, parabasal cells appear in the smear. In general, during menstruation, a woman “loses” a third of the epithelium. Also, this type of squamous epithelium cells is characteristic of the period of amenorrhea (hormonal disorders)
Basal cells with a very large nucleus are characteristic of the atrophic smear type (ATM). Diagnosed in menopausal women with at least 5 years of inactive ovaries. Also, a similar situation is observed in women with prolonged postpartum amenorrhea, if active breastfeeding continues for more than a year.
Medical terms that scare
Dystrophy or dystrophic epithelium- happens with true erosion of the cervix or pseudo-erosion, which is also called ectopia. In a word, when there is a wound on the cervix. When it heals, cell dystrophy will cease to be determined.
The cytogram often contains a medical term "metaplastic". Many people think that this indicates a malignant process. But no - metaplastic epithelium is a good smear result. It says that the cells are taken exactly from the desired zone - the junction of two types of epithelium - from endocervix (cylindrical) and exocervix (flat). This is where atypia, precancerous or cancerous changes are most often found.
Acetowhite epithelium (ABE) is not an indicator that can be displayed as a result of smears. visible with extended colposcopy after exposure to CMM with acetic acid. If there are pathological areas on it, the epithelium will begin to turn pale. Further, the doctor draws conclusions based on how quickly the whitening occurred, how bright it was, how long it lasted, whether it had borders, whether there was a sign of a ridge, etc. If the reaction was not pronounced, it is most likely that women have chronic cervicitis (inflammation ), HPV or (mild dysplasia). With rough ABE they put - severe dysplasia.
In appearance, the neck, even with severe dysplasia, can be quite healthy. And only the acetic test shows what is not visible to the eye.
Not every gynecologist is a good colposcopist. An experienced specialist monitors the cervix during an extended colposcopy after treatment with vinegar and iodine, literally without taking his eyes off, and makes very accurate diagnoses. By the way, in some countries, it is the vinegar test, and not the PAP test, that is the screening method for diagnosing precancer. If a rough acetic white epithelium is detected, the woman is taken under control and treated.
hyperplastic epithelium- is usually synonymous with a cervical canal polyp. Needs removal and histological examination.
Cells with signs of keratosis, keratinization- most often these words can be seen in the conclusions of women with suspected leukoplakia. But the same signs (features of epithelial cells) occur in precancer and cancer.
Expressed reactive changes- inflammatory process on CMM.
Signs of mild dysplasia - lsil. If there are pronounced, deep changes, we are usually talking about HSIL - severe neoplasia, in which surgical intervention is mandatory - conization of the cervix.
Koilocytosis - most characteristic of PVI (human papillomavirus, HPV). Viral defeat.
Reparative changes in the epithelium- benign cell changes, a variant of reactive changes (see above).
Degenerative changes- this is not cancer, it happens in a chronic or acute inflammatory process. In the same category, reactive changes include the following concepts: inflammatory atypia, squamous metaplasia, hyperkeratosis, parakeratosis.
Atypia, atypical changes- dysplasia (precancer) or malignancy.
Atypical squamous cells of unknown significance– . These are cells of unknown significance. The cytologist sees that they look unusual, changed, but cannot determine exactly what caused this - inflammation, infection, or irritation. You should not be afraid of this wording. It does not cause oncological alertness in the doctor. However, it is a reason for taking smears from the cervix for HPV of high oncogenic risk (mandatory types 16 and 18). And if they come to light - it is necessary to pass.
Proliferation of squamous epithelium- that is, growth or in medical terms - mitosis. Normally, this process is slow. Its meaning is to renew the upper layer of the mucous membrane of the CMM. During pregnancy, the process is more active, but normally moderate.
If, according to the results of scraping, proliferation is pronounced, then this happened for one of the following reasons:
- cervicitis (inflammatory process on the neck);
- tissue injury resulting from diagnostic curettage, abortion, difficult childbirth, conization;
- tumor growth - benign or malignant (cervical canal polyp, mild or severe dysplasia, cancer, papilloma).
That is, proliferation can be hyperplastic, inflammatory or post-traumatic.
Dyskarosis -. The cause is gynecological diseases (colpitis, cervicitis, vaginitis) or dysplasia.
When treatment is needed
- For mild dysplasia (CIN I, lsil) it is enough to observe a gynecologist, take cytological smears and colposcopy. In severe dysplasia (HSIL, CIN II, CIN III), conization is performed - surgical removal of affected tissues. In some cases, doctors decide to amputate the cervix.
- With reactive changes. Often a woman is diagnosed with the first degree of neoplasia (dysplasia) in question. Questionable because the cells can become "normal" again after antibiotic treatment.
- If found keratinization of the epithelium - leukoplakia. We wrote about this in detail. "Cauterization" of a tissue site is carried out if the presence of leukoplakia is proven by a biopsy.
- If, according to the results of a general smear on the flora, not only a large amount of squamous epithelium is noticed, but also a lot of mucus, leukocytes, and the woman herself complains of unusual discharge, itching, unpleasant odor, and so on.
The number of leukocytes in p. sp. to squamous epithelial cells
The number of leukocytes largely depends on the individual characteristics of the body and the day of the menstrual cycle (there are more of them during the period of ovulation), the presence or absence of sexual activity, and possibly chronic cervicitis - inflammation of the cervix.
For this reason, doctors do not allocate a specific rate for leukocytes. They look only at their ratio to the cells of the vaginal epithelium. The ratio of leukocytes to squamous cells should be up to 1:1. If the number of leukocytes to squamous cells increases to a ratio of 2:1, 3:1, 4:1 or more, this indicates an infection, more often about candidiasis (thrush) or trichomoniasis. 1:1 - border ratio. This is not necessarily a beginning disease. Perhaps some chemical or mechanical factor influenced the result. The same sexual intercourse if it happened a few hours before the smear. That is, 15-20 leukocytes with 15-20 epithelial cells in the field of view may be a variant of the norm. This is especially common in pregnant women.
We bring to your attention a plate from methodical recommendations for attending physicians. They show that the number of leukocytes is greater than the number of epithelial cells in nonspecific vaginitis, candidiasis, trichomoniasis. But with bacterial vaginosis, on the contrary, less.
Cytologists also pay attention to the structure of epithelial cells, their changes, the ratio of the nucleus to the cytoplasm in them. In disease, the cell nucleus is large. This is due to the fact that cells from the lower layers of the epithelium enter the scraping. And the reason for this is the active desquamation of the surface epithelium due to the inflammatory reaction.