coronary arteries. Anatomy of the coronary arteries: functions, structure and mechanism of blood supply
Read:
The widespread use of selective coronary angiography and surgical interventions on the coronary arteries of the heart in recent years has made it possible to study the anatomical features of the coronary circulation of a living person, to develop a functional anatomy of the arteries of the heart in relation to revascularization operations in patients with coronary heart disease.
Interventions on the coronary arteries for diagnostic and therapeutic purposes impose increased requirements on the study of vessels at different levels, taking into account their variants, developmental anomalies, caliber, angles of departure, possible collateral connections, as well as their projections and relationships with surrounding formations.
When systematizing these data, we paid special attention to information from the surgical anatomy of the coronary arteries, based on the principle of topographic anatomy in relation to the operation plan with the division of the coronary arteries into segments.
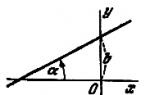
The right and left coronary arteries were conditionally divided into three and seven segments, respectively (Fig. 51).
Three segments were distinguished in the right coronary artery: I - a segment of the artery from the mouth to the outlet of the branch - the artery of the sharp edge of the heart (length from 2 to 3.5 cm); II - section of the artery from the branch of the sharp edge of the heart to the discharge of the posterior interventricular branch of the right coronary artery (length 2.2-3.8 cm); III - posterior interventricular branch of the right coronary artery.
The initial section of the left coronary artery from the mouth to the place of division into the main branches is designated as segment I (length from 0.7 to 1.8 cm). The first 4 cm of the anterior interventricular branch of the left coronary artery is divided
Rice. 51. Segmental division of the coronary
heart arteries:
BUT- right coronary artery; B- left coronary artery
into two segments of 2 cm each - II and III segments. The distal portion of the anterior interventricular branch was segment IV. The circumflex branch of the left coronary artery to the point of origin of the branch of the blunt edge of the heart is the V segment (length 1.8-2.6 cm). The distal section of the circumflex branch of the left coronary artery was more often represented by the artery of the obtuse margin of the heart - segment VI. And, finally, the diagonal branch of the left coronary artery is the VII segment.
The use of segmental division of the coronary arteries, as our experience has shown, is advisable in a comparative study of the surgical anatomy of the coronary circulation according to selective coronary angiography and surgical interventions, to determine the localization and spread of the pathological process in the arteries of the heart, and is of practical importance when choosing the method of surgical intervention in the case of coronary disease hearts. 
Rice. 52. Right-wing type of coronary circulation. Well developed posterior interventricular branches
Beginning of the coronary arteries . Sinuses of the aorta, from which the coronary arteries depart, James (1961) proposes to call the right and left coronary sinus. The orifices of the coronary arteries are located in the bulb of the ascending aorta at the level of the free edges of the aortic semilunar valves or 2-3 cm above or below them (V. V. Kovanov and T. I. Anikina, 1974).
The topography of the sections of the coronary arteries, as A. S. Zolotukhin (1974) points out, is different and depends on the structure of the heart and chest. According to M. A. Tikhomirov (1899), the orifices of the coronary arteries in the aortic sinuses can be located below the free edge of the valves "abnormally low", so that the semilunar valves pressed against the wall of the aorta close the orifices, either at the level of the free edge of the valves, or above them, by wall of the ascending aorta.
The level of the location of the mouths is of practical importance. With a high location at the time of left ventricular systole, the orifice is
under the blow of a stream of blood, not being covered by the edge of the semilunar valve. According to A. V. Smolyannikov and T. A. Naddachina (1964), this may be one of the reasons for the development of coronary sclerosis.
The right coronary artery in most patients has a main type of division and plays an important role in the vascularization of the heart, especially its posterior diaphragmatic surface. In 25% of patients in the blood supply to the myocardium, we revealed the predominance of the right coronary artery (Fig. 52). N. A. Javakhshivili and M. G. Komakhidze (1963) describe the beginning of the right coronary artery in the region of the anterior right sinus of the aorta, indicating that its high discharge is rarely observed. The artery enters the coronary sulcus, located behind the base of the pulmonary artery and under the auricle of the right atrium. The section of the artery from the aorta to the sharp edge of the heart (segment I of the artery) is adjacent to the wall of the heart and is completely covered by subepicardial fat. The diameter of segment I of the right coronary artery ranges from 2.1 to 7 mm. Along the artery trunk on the anterior surface of the heart in the coronary sulcus, epicardial folds are formed, filled with adipose tissue. Abundantly developed adipose tissue is noted along the artery from the sharp edge of the heart. The atherosclerotically altered trunk of the artery along this length is well palpated in the form of a cord. Detection and isolation of segment I of the right coronary artery on the anterior surface of the heart is usually not difficult.
The first branch of the right coronary artery - the artery of the arterial cone, or the fatty artery - leaves directly at the beginning of the coronary sulcus, continuing down to the right at the arterial cone, giving branches to the cone and the wall of the pulmonary trunk. In 25.6% of patients, we observed its common beginning with the right coronary artery, its mouth was located at the mouth of the right coronary artery. In 18.9% of patients, the mouth of the conus artery was located next to the mouth of the coronary artery, located behind the latter. In these cases, the vessel originated directly from the ascending aorta and was only slightly inferior in size to the trunk of the right coronary artery.
Muscular branches depart from the I segment of the right coronary artery to the right ventricle of the heart. Vessels in the amount of 2-3 are located closer to the epicardium in connective tissue couplings on the layer of adipose tissue covering the epicardium.
The other most significant and permanent branch of the right coronary artery is the right marginal artery (a branch of the sharp edge of the heart). The artery of the acute edge of the heart, a constant branch of the right coronary artery, departs in the region of the acute edge of the heart and descends along the lateral surface of the heart to its apex. It supplies blood to the anterior-lateral wall of the right ventricle, and sometimes to the diaphragmatic part of it. In some patients, the diameter of the lumen of the artery was about 3 mm, but more often it was 1 mm or less.
Continuing along the coronary sulcus, the right coronary artery goes around the sharp edge of the heart, passes to the posterior diaphragmatic surface of the heart and ends to the left of the posterior interventricular sulcus, not reaching the blunt edge of the heart (in 64% of patients).
The final branch of the right coronary artery - the posterior interventricular branch (III segment) - is located in the posterior interventricular groove, descending along it to the apex of the heart. V. V. Kovanov and T. I. Anikina (1974) distinguish three variants of its distribution: 1) in the upper part of the furrow of the same name; 2) throughout this groove to the top of the heart; 3) the posterior interventricular branch enters the anterior surface of the heart. According to our data, only in 14% of patients it reached
apex of the heart, anastomosing with the anterior interventricular branch of the left coronary artery.
From the posterior interventricular branch into the interventricular septum at right angles, from 4 to 6 branches depart, supplying blood to the conducting system of the heart.
With a right-sided type of coronary blood supply to the diaphragmatic surface of the heart, 2-3 muscle branches extend from the right coronary artery, running parallel to the posterior interventricular branch of the right coronary artery.
To access the II and III segments of the right coronary artery, it is necessary to lift the heart up and take it to the left. II segment of the artery is located superficially in the coronary sulcus; it can be easily and quickly found and selected. The posterior interventricular branch (III segment) is located deep in the interventricular groove and is covered by subepicardial fat. When performing operations on the II segment of the right coronary artery, it must be remembered that the wall of the right ventricle in this place is very thin. Therefore, it should be handled carefully to avoid perforation.
The left coronary artery, participating in the blood supply to most of the left ventricle, the interventricular septum, as well as the anterior surface of the right ventricle, dominates the blood supply to the heart in 20.8% of patients. Starting in the left sinus of Valsalva, it goes from the ascending aorta to the left and down the coronary sulcus of the heart. The initial section of the left coronary artery (I segment) before the bifurcation has a length of at least 8 mm and not more than 18 mm. Isolation of the main trunk of the left coronary artery is difficult, since it is hidden by the root of the pulmonary artery.
The short trunk of the left coronary artery, 3.5 to 7.5 mm in diameter, turns to the left between the pulmonary artery and the base of the left auricle of the heart and divides into the anterior interventricular and circumflex branches. (II, III, IV segments of the left coronary artery) is located in the anterior interventricular groove of the heart, along which it goes to the apex of the heart. It can end at the apex of the heart, but usually (according to our observations, in 80% of patients) it continues on the diaphragmatic surface of the heart, where it meets the terminal branches of the posterior interventricular branch of the right coronary artery and participates in the vascularization of the diaphragmatic surface of the heart. The diameter of segment II of the artery ranges from 2 to 4.5 mm.
It should be noted that a significant part of the anterior interventricular branch (segments II and III) lies deep, covered by subepicardial fat and muscle bridges. The isolation of the artery in this place requires great care because of the danger of possible damage to its muscular and, most importantly, septal branches leading to the interventricular septum. The distal part of the artery (IV segment) is usually located superficially, is clearly visible under a thin layer of subepicardial tissue and is easily distinguished.
From the II segment of the left coronary artery, from 2 to 4 septal branches extend deep into the myocardium, which are involved in the vascularization of the interventricular septum of the heart.
Throughout the anterior interventricular branch of the left coronary artery, 4-8 muscle branches depart to the myocardium of the left and right ventricles. The branches to the right ventricle are smaller in caliber than to the left, although they are the same in size as the muscular branches from the right coronary artery. A significantly larger number of branches extend to the anterior-lateral wall of the left ventricle. In functional terms, the diagonal branches are especially important (there are 2 of them, sometimes 3), extending from the II and III segments of the left coronary artery.
When searching for and isolating the anterior interventricular branch, an important landmark is the large vein of the heart, which is located in the anterior interventricular groove to the right of the artery and is easily found under a thin layer of the epicardium.
The circumflex branch of the left coronary artery (V-VI segments) departs at a right angle to the main trunk of the left coronary artery, located in the left coronary sulcus, under the left auricle of the heart. Its permanent branch - the branch of the blunt edge of the heart - descends over a considerable distance at the left edge of the heart, somewhat backwards, and in 47.2% of patients reaches the apex of the heart.
After the branches branch off to the blunt edge of the heart and the posterior surface of the left ventricle, the circumflex branch of the left coronary artery in 20% of patients continues along the coronary sulcus or along the posterior wall of the left atrium in the form of a thin trunk and reaches the confluence of the inferior posterior vein.
The V segment of the artery is easily detected, which is located in the fatty membrane under the ear of the left atrium and is covered by a large vein of the heart. The latter sometimes has to be crossed to gain access to the trunk of the artery.
The distal section of the circumflex branch (VI segment) is usually located on the posterior surface of the heart and, if necessary, surgical intervention on it, the heart is lifted and retracted to the left while simultaneously retracting the left ear of the heart.
The diagonal branch of the left coronary artery (VII segment) goes along the anterior surface of the left ventricle down and to the right, then plunging into the myocardium. The diameter of its initial part is from 1 to 3 mm. With a diameter of less than 1 mm, the vessel is little expressed and is more often considered as one of the muscular branches of the anterior interventricular branch of the left coronary artery.
Anatomy of the coronary arteries

coronary arteries
From an anatomical point of view, the coronary artery system is divided into two parts - right and left. From a surgical standpoint, the coronary artery is divided into four parts: the left main coronary artery (trunk), the left anterior descending artery or anterior interventricular branch (LAD) and its branches, the left circumflex coronary artery (OC) and its branches, the right coronary artery (RCA) ) and its branches.
The large coronary arteries form an arterial ring and loop around the heart. The left circumflex and right coronary arteries are involved in the formation of the arterial ring, passing through the atrioventricular sulcus. The formation of the arterial loop of the heart involves the anterior descending artery from the system of the left coronary artery and the posterior descending artery from the system of the right coronary artery, or from the system of the left coronary artery - from the left circumflex artery with the left dominant type of blood supply. The arterial ring and loop are a functional device for the development of collateral circulation of the heart.
Right coronary artery
The right coronary artery (right coronary artery) departs from the right sinus of Valsalva and passes in the coronary (atrioventricular) groove. In 50% of cases, immediately at the place of origin, it gives off the first branch - the branch of the arterial cone (conus artery, conus branch, CB), which feeds the infundibulum of the right ventricle. Its second branch is the artery of the sinoatrial node (S-A node artery, SNA). leaving from the right coronary artery back at a right angle into the gap between the aorta and the wall of the right atrium, and then along its wall to the sinoatrial node. As a branch of the right coronary artery, this artery occurs in 59% of cases. In 38% of cases, the artery of the sinoatrial node is a branch of the left circumflex artery. And in 3% of cases there is a blood supply to the sino-atrial node from two arteries (both from the right and from the circumflex). In the anterior part of the coronary sulcus, in the region of the acute edge of the heart, the right marginal branch departs from the right coronary artery (acute marginal artery, acute marginal branch, AMB), more often from one to three, which in most cases reaches the apex of the heart. Then the artery turns back, lies in the back of the coronary sulcus and reaches the "cross" of the heart (the intersection of the posterior interventricular and atrioventricular sulcus of the heart).
With the so-called right type of blood supply to the heart, observed in 90% of people, the right coronary artery gives off the posterior descending artery (PDA), which runs along the posterior interventricular groove for a different distance, giving branches to the septum (anastomosing with similar branches from the anterior descending artery, the latter usually longer than the first), the right ventricle and branches to the left ventricle. After the posterior descending artery (PDA) originates, the RCA continues beyond the cross of the heart as the right posterior atrioventricular branch along the distal part of the left atrioventricular sulcus, terminating in one or more posterolateral branches (posterolateral branches) feeding the diaphragmatic surface of the left ventricle. . On the posterior surface of the heart, immediately below the bifurcation, at the point of transition of the right coronary artery into the posterior interventricular sulcus, an arterial branch originates from it, which, piercing the interventricular septum, goes to the atrioventricular node - the artery of the atrioventricular node (atrioventricular node artery, AVN).
Left coronary artery
The left coronary artery (left coronary artery) starts from the left posterior surface of the aortic bulb and goes to the left side of the coronary sulcus. Its main trunk (left main coronary artery, LMCA) is usually short (0-10 mm, diameter varies from 3 to 6 mm) and is divided into anterior interventricular (left anterior descending artery, LAD) and envelope (left circumflex artery, LCx) branches . In 30-37% of cases, the third branch departs here - the intermediate artery (ramus intermedius, RI), which crosses obliquely the wall of the left ventricle. LAD and OB form an angle between them, which varies from 30 to 180°.
Anterior interventricular branch
The anterior interventricular branch is located in the anterior interventricular sulcus and goes to the apex, giving off the anterior ventricular branches (diagonal, diagonal artery, D) and the anterior septal (septal branch)) along the way. In 90% of cases, one to three diagonal branches are determined. Septal branches depart from the anterior interventricular artery at an angle of approximately 90 degrees, perforate the interventricular septum, feeding it. The anterior interventricular branch sometimes enters the thickness of the myocardium and again lies in the groove and often reaches the apex of the heart along it, where in about 78% of people it turns back to the diaphragmatic surface of the heart and for a short distance (10-15 mm) rises up along the posterior interventricular groove. In such cases, it forms a posterior ascending branch. Here it often anastomoses with the terminal branches of the posterior interventricular artery, a branch of the right coronary artery.
circumflex artery
Anatomy of the coronary arteries.
Professor, Dr. med. Sciences Yu.P. Ostrovsky
At the moment, there are many options for the classification of coronary arteries adopted in different countries and centers of the world. But, in our opinion, there are certain terminological differences between them, which creates difficulties in the interpretation of coronary angiography data by specialists of different profiles.
We have analyzed the literature on the anatomy and classification of the coronary arteries. Data from literary sources are compared with their own. A working classification of the coronary arteries has been developed in accordance with the nomenclature adopted in the English literature.
coronary arteries
From an anatomical point of view, the coronary artery system is divided into two parts - right and left. From a surgical standpoint, the coronary artery is divided into four parts: the left main coronary artery (trunk), the left anterior descending artery or anterior interventricular branch (LAD) and its branches, the left circumflex coronary artery (OC) and its branches, the right coronary artery (RCA) ) and its branches.
The large coronary arteries form an arterial ring and loop around the heart. The left circumflex and right coronary arteries are involved in the formation of the arterial ring, passing through the atrioventricular sulcus. The anterior descending artery from the system of the left coronary artery and the posterior descending artery from the system of the right coronary artery, or from the system of the left coronary artery - from the left circumflex artery with the left dominant type of blood supply participate in the formation of the arterial loop of the heart. The arterial ring and loop are a functional device for the development of collateral circulation of the heart.
Right coronary artery
Right coronary artery(right coronary artery) departs from the right sinus of Valsalva and passes in the coronary (atrioventricular) groove. In 50% of cases, immediately at the place of origin, it gives off the first branch - the branch of the arterial cone (conus artery, conus branch, CB), which feeds the infundibulum of the right ventricle. Its second branch is the artery of the sinoatrial node (S-A node artery, SNA). leaving the right coronary artery back at a right angle into the gap between the aorta and the wall of the right atrium, and then along its wall to the sinoatrial node. As a branch of the right coronary artery, this artery occurs in 59% of cases. In 38% of cases, the artery of the sinoatrial node is a branch of the left circumflex artery. And in 3% of cases there is a blood supply to the sino-atrial node from two arteries (both from the right and from the circumflex). In the anterior part of the coronary sulcus, in the region of the acute edge of the heart, the right marginal branch departs from the right coronary artery (acute marginal artery, acute marginal branch, AMB), more often from one to three, which in most cases reaches the apex of the heart. Then the artery turns back, lies in the back of the coronary sulcus and reaches the "cross" of the heart (the intersection of the posterior interventricular and atrioventricular sulcus of the heart).
With the so-called right type of blood supply to the heart, observed in 90% of people, the right coronary artery gives off the posterior descending artery (PDA), which runs along the posterior interventricular groove for a different distance, giving branches to the septum (anastomosing with similar branches from the anterior descending artery, the latter usually longer than the first), the right ventricle and branches to the left ventricle. After the posterior descending artery (PDA) originates, the RCA continues beyond the cross of the heart as the right posterior atrioventricular branch along the distal part of the left atrioventricular sulcus, terminating in one or more posterolateral branches (posterolateral branches) feeding the diaphragmatic surface of the left ventricle. . On the posterior surface of the heart, immediately below the bifurcation, at the point of transition of the right coronary artery into the posterior interventricular sulcus, an arterial branch originates from it, which, piercing the interventricular septum, goes to the atrioventricular node - the artery of the atrioventricular node artery (AVN).
The branches of the right coronary artery vascularize: the right atrium, part of the anterior, the entire posterior wall of the right ventricle, a small portion of the posterior wall of the left ventricle, the interatrial septum, the posterior third of the interventricular septum, the papillary muscles of the right ventricle and the posterior papillary muscle of the left ventricle.
Left coronary artery
Left coronary artery(left coronary artery) starts from the left posterior surface of the aortic bulb and goes to the left side of the coronary sulcus. Its main trunk (left main coronary artery, LMCA) is usually short (0-10 mm, diameter varies from 3 to 6 mm) and is divided into anterior interventricular (left anterior descending artery, LAD) and envelope (left circumflex artery, LCx) branches . In 30-37% of cases, the third branch departs here - the intermediate artery (ramus intermedius, RI), which crosses obliquely the wall of the left ventricle. LAD and OB form an angle between them, which varies from 30 to 180°.
Anterior interventricular branch
The anterior interventricular branch is located in the anterior interventricular sulcus and goes to the apex, giving off the anterior ventricular branches (diagonal, diagonal artery, D) and the anterior septal (septal branch)) along the way. In 90% of cases, one to three diagonal branches are determined. Septal branches depart from the anterior interventricular artery at an angle of approximately 90 degrees, perforate the interventricular septum, feeding it. The anterior interventricular branch sometimes enters the thickness of the myocardium and again lies in the groove and often reaches the apex of the heart along it, where in about 78% of people it turns back to the diaphragmatic surface of the heart and for a short distance (10-15 mm) rises up along the posterior interventricular groove. In such cases, it forms a posterior ascending branch. Here it often anastomoses with the terminal branches of the posterior interventricular artery, a branch of the right coronary artery.
The circumflex branch of the left coronary artery is located in the left part of the coronary sulcus and in 38% of cases gives the first branch to the artery of the sinoatrial node, and then the artery of the obtuse marginal artery (obtuse marginal artery, obtuse marginal branch, OMB), usually from one to three. These fundamentally important arteries feed the free wall of the left ventricle. In the case when there is a right type of blood supply, the circumflex branch gradually becomes thinner, giving branches to the left ventricle. With a relatively rare left type (10% of cases), it reaches the level of the posterior interventricular sulcus and forms the posterior interventricular branch. With an even rarer, so-called mixed type, there are two posterior ventricular branches of the right coronary and from the circumflex arteries. The left circumflex artery forms important atrial branches, which include the left atrial circumflex artery (LAC) and the large anastomosing auricular artery.
The branches of the left coronary artery vascularize the left atrium, the entire anterior and most of the posterior wall of the left ventricle, part of the anterior wall of the right ventricle, the anterior 2/3 of the interventricular septum, and the anterior papillary muscle of the left ventricle.
Types of blood supply to the heart
The type of blood supply to the heart is understood as the predominant distribution of the right and left coronary arteries on the posterior surface of the heart.
The anatomical criterion for assessing the predominant type of distribution of the coronary arteries is the avascular zone on the posterior surface of the heart, formed by the intersection of the coronary and interventricular sulci, - crux. Depending on which of the arteries - right or left - reaches this zone, the predominant right or left type of blood supply to the heart is distinguished. The artery reaching this zone always gives off a posterior interventricular branch, which runs along the posterior interventricular sulcus towards the apex of the heart and supplies blood to the posterior part of the interventricular septum. Another anatomical feature is described to determine the predominant type of blood supply. It is noted that the branch to the atrioventricular node always departs from the predominant artery, i.e. from the artery, which is of the greatest importance in the supply of blood to the posterior surface of the heart.
Thus, with predominant right type of blood supply to the heart The right coronary artery supplies the right atrium, the right ventricle, the posterior part of the interventricular septum, and the posterior surface of the left ventricle. The right coronary artery is represented by a large trunk, and the left circumflex artery is poorly expressed.
With predominant left type of blood supply to the heart the right coronary artery is narrow and terminates in short branches on the diaphragmatic surface of the right ventricle, and the posterior surface of the left ventricle, the posterior part of the interventricular septum, the atrioventricular node and most of the posterior surface of the ventricle receive blood from the well-defined large left circumflex artery.
In addition, there are also balanced type of blood supply. in which the right and left coronary arteries contribute approximately equally to the blood supply to the posterior surface of the heart.
The concept of "primary type of blood supply to the heart", although conditional, is based on the anatomical structure and distribution of the coronary arteries in the heart. Since the mass of the left ventricle is much larger than the right one, and the left coronary artery always supplies blood to most of the left ventricle, 2/3 of the interventricular septum and the wall of the right ventricle, it is clear that the left coronary artery is predominant in all normal hearts. Thus, in any type of coronary blood supply, the left coronary artery is predominant in the physiological sense.
Nevertheless, the concept of "predominant type of blood supply to the heart" is valid, it is used to assess anatomical findings during coronary angiography and is of great practical importance in determining indications for myocardial revascularization.
For topical indication of lesions, it is proposed to divide the coronary bed into segments.
Dotted lines in this scheme highlight the segments of the coronary arteries.
So in the left coronary artery in the anterior interventricular branch it is divided into three segments:
1. proximal - from the place of origin of the LAD from the trunk to the first septal perforator or 1DV.
2. medium - from 1DV to 2DV.
3. distal - after the discharge of 2DV.
In circumflex artery It is also customary to distinguish three segments:
1. proximal - from the mouth of the OB to 1 VTK.
3. distal - after the departure of 3 VTK.
Right coronary artery divided into the following main segments:
1. proximal - from the mouth to 1 wok
2. medium - from 1 wok to the sharp edge of the heart
3. distal - up to the RCA bifurcation to the posterior descending and posterolateral arteries.
Coronary angiography
Coronary angiography(coronary angiography) is an X-ray visualization of the coronary vessels after the introduction of a radiopaque substance. The x-ray image is immediately recorded on 35 mm film or digital media for further analysis.
Currently, coronary angiography is the "gold standard" for determining the presence or absence of stenosis in coronary disease.
The purpose of coronary angiography is to determine the coronary anatomy and the degree of narrowing of the lumen of the coronary arteries. Information obtained during the procedure includes determining the location, extent, diameter and contours of the coronary arteries, the presence and degree of coronary obstruction, characterization of the nature of the obstruction (including the presence of an atherosclerotic plaque, thrombus, dissection, spasm or myocardial bridge).
The data obtained determine the further tactics of the patient's treatment: coronary bypass grafting, intervention, drug therapy.
To conduct high-quality angiography, selective catheterization of the right and left coronary arteries is necessary, for which a large number of diagnostic catheters of various modifications have been created.
The study is performed under local anesthesia and NLA through arterial access. The following arterial accesses are generally recognized: femoral arteries, brachial arteries, radial arteries. Transradial access has recently gained a strong position and has become widely used due to its low trauma and convenience.
After puncture of the artery, diagnostic catheters are inserted through the introducer, followed by selective catheterization of the coronary vessels. The contrast agent is dosed using an automatic injector. Shooting is performed in standard projections, the catheters and intraduser are removed, and a compression bandage is applied.
Basic angiographic projections
During the procedure, the goal is to obtain the most complete information about the anatomy of the coronary arteries, their morphological characteristics, the presence of changes in the vessels with an accurate determination of the location and nature of the lesions.
To achieve this goal, coronary angiography of the right and left coronary arteries is performed in standard projections. (Their description is given below). If it is necessary to conduct a more detailed study, shooting is carried out in special projections. This or that projection is optimal for the analysis of a certain section of the coronary bed and allows you to most accurately identify the features of the morphology and the presence of pathology in this segment.
Below are the main angiographic projections with an indication of the arteries for visualization of which these projections are optimal.
For left coronary artery There are the following standard projections.
1. Right anterior oblique with caudal angulation.
RAO 30, Caudal 25.
2. Right anterior oblique view with cranial angulation.
RAO 30, cranial 20
LAD, its septal and diagonal branches
3. Left anterior oblique with cranial angulation.
LAO 60, cranial 20.
Orifice and distal segment of the LCA trunk, middle and distal segment of the LAD, septal and diagonal branches, proximal segment of the OB, VTK.
The heart is a muscular organ that circulates blood around the body like a pump. The heart is provided with autonomous innervation, which determines the involuntary, rhythmic work of the muscle layer of the organ - the myocardium. In addition to nerve structures, the heart also has its own blood supply system.
Most of us know that the human cardiovascular system consists of two main circles of blood circulation: large and small. However, specialists in cardiology consider the vascular system that feeds the tissues of the heart as a third or coronary circle of blood circulation.
If we consider a three-dimensional model of the heart with the vessels that feed it, we can see that a network of arteries and veins surrounds the heart like a wreath or crown. Hence the name of this circulatory system - the coronary or coronary circle.

The coronary circle of hemocirculation is made up of vessels, the structure of which does not fundamentally differ from other vessels of the body. The vessels that carry oxygenated blood to the myocardium are called coronary arteries. Vessels that provide outflow of deoxygenated, i.e. venous blood are the coronary veins. About 10% of all blood passing through the aorta enters the coronary vessels. The anatomy of the vessels of the coronary circle of hemocirculation is different for each person and is individual.
Schematically, the coronary circulation can be expressed as follows: aorta - coronary arteries - arterioles - capillaries - venules - coronary veins - right atrium.
Consider the scheme of hemocirculation in the coronary circle in stages.
arteries
The coronary arteries branch off from the so-called sinuses of Valsalva. This is the dilated portion of the aortic root just above the valve.
The sinuses are named according to the arteries coming out of them, i.e. the right sinus gives rise to the right artery, the left sinus gives rise to the left artery. The right one passes along the coronary sulcus on the right, then stretches back and to the top of the heart. Along the branches extending from this highway, the blood rushes into the thickness of the myocardium of the right ventricle, washes the tissues of the posterior part of the left ventricle and a significant proportion of the cardiac septum.

The left coronary artery, leaving the aorta, is divided into 2, and sometimes 3 or 4 vessels. One of them - ascending, passes along the groove that separates the ventricles, in front. Multiple small vessels extending from this branch provide blood flow to the anterior walls of both ventricles. Another vessel, descending, passes along the coronal sulcus on the left. This highway carries enriched blood to the tissues of the atrium and ventricle on the left.
Further, the artery goes around the heart on the left and rushes to its apex, where it forms an anastomosis - the fusion of the right cardiac artery and the descending branch of the left. In the course of the descending anterior artery, smaller vessels branch off, providing blood to the anterior region of the myocardium of the left and right ventricles.
4% of the population has a third coronary artery. An even rarer case is when a person has only one heart artery.
Feedback from our reader - Alina Mezentseva
I recently read an article that talks about the natural cream "Bee Spas Chestnut" for the treatment of varicose veins and cleaning blood vessels from blood clots. With the help of this cream, you can FOREVER cure VARICOSIS, eliminate pain, improve blood circulation, increase the tone of the veins, quickly restore the walls of blood vessels, clean and restore varicose veins at home.
I was not used to trusting any information, but I decided to check and ordered one package. I noticed the changes in a week: the pain went away, the legs stopped "buzzing" and swelling, and after 2 weeks the venous cones began to decrease. Try it and you, and if anyone is interested, then below is a link to the article.
Also sometimes there is a doubling of the cardiac arterial trunks. In this case, instead of one arterial trunk, two parallel vessels go to the heart.

The coronary arteries are characterized by partial autonomy, expressed in the fact that they are able to independently maintain the required level of blood flow in the myocardium. This functional feature of the coronary arteries is extremely important, because. The heart is an organ that works constantly, continuously. That is why a violation of the state of the heart arteries (atherosclerosis, stenosis) can lead to fatal consequences.
Vienna
"Spent", i.e. saturated with carbon dioxide and other products of tissue metabolism, blood from the tissues of the heart drains into the coronary veins.
 The large coronal vein begins at the apex of the heart, runs along the anterior (ventral) interventricular sulcus, turns left along the coronary sulcus, rushes back and flows into the coronary sinus.
The large coronal vein begins at the apex of the heart, runs along the anterior (ventral) interventricular sulcus, turns left along the coronary sulcus, rushes back and flows into the coronary sinus.
This is a venous structure, about 3 cm in size, located on the posterior (dorsal) part of the heart in the coronary sulcus, has an outlet in the cavity of the right atrium, the mouth does not exceed 12 mm in diameter. The structure is considered to be part of a large vein.
The middle coronary vein exits at the apex of the heart, next to the great vein, but runs along the dorsal interventricular sulcus. The middle vein also empties into the coronary sinus.

For the treatment of VARICOSIS and cleaning blood vessels from blood clots, Elena Malysheva recommends a new method based on Cream of Varicose Veins cream. It contains 8 useful medicinal plants that are extremely effective in the treatment of VARICOSIS. In this case, only natural ingredients are used, no chemicals and hormones!
The small coronary vein is located in the groove separating the right ventricle and atrium from each other, usually passes into the middle vein, and sometimes directly into the coronary sinus.
In the oblique cardiac vein, blood is collected from the posterior region of the myocardium of the left atrium. Through the posterior vein, venous blood flows from the tissues of the posterior wall of the left ventricle. These are small vessels that also empty into the coronary sinus.

There are also anterior and small cardiac veins, which have independent exits into the cavity of the right atrium. The anterior veins carry out the outflow of venous blood from the thickness of the muscular layer of the right ventricle. The small veins drain blood from the intracavitary tissues of the heart.
Blood flow rate
As mentioned above, coronary vessels have individual anatomical features for each person. The limits of the norm are quite wide, if we are not talking about serious anomalies of the structure, when the vital activity of the heart suffers to a large extent.
In cardiology, there is such a thing as blood flow dominance, an indicator that determines which arteries give off the posterior descending (or interventricular) artery.
If the supply of the posterior interventricular branch occurs due to the right and one of the branches of the left arteries, they speak of codominance - 20% of the population is typical. In this case, there is a uniform nutrition of the myocardium. The most common right type of dominance is inherent in 70% of the population.

In this variant, the dorsal descending artery arises from the right coronary artery. Only 10% of the population has a left type of blood flow dominance. In this case, the posterior descending artery branches off from one of the branches of the left coronary artery. With right and left dominance of blood flow, uneven blood supply to the heart muscle occurs.
 The intensity of cardiac blood flow is unstable. So, at rest, the blood flow rate is 60-70 mg/min per 100 g of myocardium. During exercise, the speed increases 4-5 times and depends on the general condition of the heart muscle, the degree of its endurance, the frequency of heart contractions, the characteristics of the functioning of the nervous system of a given person, and aortic pressure.
The intensity of cardiac blood flow is unstable. So, at rest, the blood flow rate is 60-70 mg/min per 100 g of myocardium. During exercise, the speed increases 4-5 times and depends on the general condition of the heart muscle, the degree of its endurance, the frequency of heart contractions, the characteristics of the functioning of the nervous system of a given person, and aortic pressure.
Interestingly, during systolic contraction of the myocardium, the movement of blood in the heart practically stops. This is a consequence of the powerful compression of all vessels by the muscular layer of the heart. With diastolic relaxation of the myocardium, blood flow in the vessels resumes.
The heart is a unique organ. Its uniqueness lies in the almost complete autonomy of its work. Thus, the heart has not only an individual hemocirculation system, but also its own nervous structures that set the rhythm of its contractions. Therefore, it is necessary to create conditions for maintaining the health of all systems that ensure the full functioning of this important organ.
DO YOU STILL THINK IT IS IMPOSSIBLE TO GET RID OF VARICOSIS!?
Have you ever tried to get rid of VARICOSIS? Judging by the fact that you are reading this article, the victory was not on your side. And of course, you know firsthand what it is:
- feeling of heaviness in the legs, tingling ...
- swelling of the legs, worse in the evening, swollen veins...
- bumps on the veins of the arms and legs ...
Now answer the question: does it suit you? Can ALL THESE SYMPTOMS be tolerated? And how much effort, money and time have you already "leaked" for ineffective treatment? After all, sooner or later the SITUATION WILL aggravate and the only way out will be only surgical intervention!
That's right - it's time to start ending this problem! Do you agree? That is why we decided to publish an exclusive interview with the head of the Institute of Phlebology of the Ministry of Health of the Russian Federation - V. M. Semenov, in which he revealed the secret of a penny method of treating varicose veins and complete restoration of blood vessels. Read interview...
The heart is the most important organ for maintaining the life of the human body. Through its rhythmic contractions, it carries the blood throughout the body, providing nourishment to all the elements.
The coronary arteries are responsible for supplying oxygen to the heart.. Another common name for them is coronary vessels.
The cyclical repetition of this process ensures uninterrupted blood supply, which keeps the heart in working condition.Coronaries are a whole group of vessels that supply blood to the heart muscle (myocardium). They carry oxygen-rich blood to all parts of the heart.
The outflow, depleted of its content (venous) blood, is carried out by 2/3 of the large vein, medium and small, which are woven into a single extensive vessel - the coronary sinus. The remainder is excreted by the anterior and Tebezian veins.
When the heart ventricles contract, the shutter closes off the arterial valve. The coronary artery at this point is almost completely blocked and blood circulation in this area stops.
The flow of blood resumes after the opening of the entrances to the arteries. The filling of the sinuses of the aorta occurs due to the impossibility of returning blood to the cavity of the left ventricle, after its relaxation, because. at this time, the dampers are closed.
Important! The coronary arteries are the only possible source of blood supply for the myocardium, so any violation of their integrity or mechanism of operation is very dangerous.
Scheme of the structure of the vessels of the coronary bed
The structure of the coronary network has a branched structure: several large branches and many smaller ones.
Arterial branches originate from the aortic bulb, immediately after the valve of the aortic valve and, bending around the surface of the heart, carry out blood supply to its different departments.
These vessels of the heart consist of three layers:
- Initial - endothelium;
- Muscular fibrous layer;
- Adventitia.
This layering makes the walls of the vessels very elastic and durable.. This contributes to proper blood flow even under conditions of high stress on the cardiovascular system, including during intense sports, which increase the speed of blood movement up to five times.
Types of coronary arteries
All vessels that make up a single arterial network, based on the anatomical details of their location, are divided into:
- Basic (epicardial)
- Adnexal (other branches):
- Right coronary artery. Its main duty is to feed the right heart ventricle. Partially supplies oxygen to the wall of the left heart ventricle and the common septum.
- Left coronary artery. Provides blood flow to all other cardiac departments. It is a branching into several parts, the number of which depends on the personal characteristics of a particular organism.
- envelope branch. It is a branch from the left side and feeds the septum of the corresponding ventricle. It is subject to increased thinning in the presence of the slightest damage.
- Anterior descending(large interventricular) branch. It also comes from the left artery. It forms the basis for the supply of nutrients to the heart and the septum between the ventricles.
- subendocardial arteries. They are considered part of the overall coronary system, but run deep within the heart muscle (myocardium) rather than on the surface itself.
 All arteries are located directly on the surface of the heart itself (except for subendocardial vessels). Their work is regulated by their own internal processes, which also control the exact volume of blood supplied to the myocardium.
All arteries are located directly on the surface of the heart itself (except for subendocardial vessels). Their work is regulated by their own internal processes, which also control the exact volume of blood supplied to the myocardium. Variants of dominant blood supply
Dominant, feeding the posterior descending branch of the artery, which can be either right or left.
Determine the general type of blood supply to the heart:
- The right blood supply is dominant if this branch departs from the corresponding vessel;
- The left type of nutrition is possible if the posterior artery is a branch from the circumflex vessel;
- The blood flow can be considered balanced if it comes simultaneously from the right trunk and from the circumflex branch of the left coronary artery.
Reference. The predominant source of nutrition is determined on the basis of the total flow of blood flow to the atrioventricular node.
In the vast majority of cases (about 70%), a dominant right blood supply is observed in a person. Equivalent work of both arteries is present in 20% of people. Left dominant nutrition through the blood is manifested only in the remaining 10% of cases.
What is coronary heart disease?
Ischemic heart disease (CHD), also called coronary heart disease (CHD), is any disease associated with a sharp deterioration in the blood supply to the heart, due to insufficient activity of the coronary system.
 IHD can be either acute or chronic.
IHD can be either acute or chronic. Most often, it manifests itself against the background of atherosclerosis of the arteries, which occurs due to a general thinning or violation of the integrity of the vessel.
A plaque is formed at the site of damage, which gradually increases in size, narrows the lumen and thereby prevents the normal flow of blood.
The list of coronary diseases includes:
- angina;
- Arrhythmia;
- Embolism;
- Arteritis;
- heart attack;
- Distortion of the coronary arteries;
- Death due to cardiac arrest.
Coronary disease is characterized by undulating jumps in the general condition, in which the chronic phase rapidly passes into the acute phase and vice versa.
How pathologies are determined
Coronary diseases are manifested by severe pathologies, the initial form of which is angina pectoris. Subsequently, it develops into more serious diseases, and strong nervous or physical stress is no longer required for the onset of attacks.
angina pectoris
 Scheme of changes in the coronary artery
Scheme of changes in the coronary artery In everyday life, such a manifestation of IHD is sometimes called "toad on the chest." This is due to the occurrence of asthma attacks, which are accompanied by pain.
Initially, symptoms begin in the chest area, after which they spread to the left back, shoulder blade, collarbone and lower jaw (rarely).
Pain is the result of oxygen starvation of the myocardium, the aggravation of which occurs in the process of physical, mental work, excitement or overeating.
myocardial infarction
Cardiac infarction is a very serious condition, accompanied by the death of certain parts of the myocardium (necrosis). This is due to a continuous cessation or incomplete flow of blood into the organ, which, most often, occurs against the background of the formation of a blood clot in the coronary vessels.
 blockage of a coronary artery
blockage of a coronary artery - Sharp pain in the chest, which is given to neighboring areas;
- Heaviness, tightness of breath;
- Trembling, muscle weakness, sweating;
- Coronary pressure is greatly reduced;
- Attacks of nausea, vomiting;
- Fear, sudden panic attacks.
The part of the heart that has undergone necrosis does not perform its functions, and the remaining half continues its work in the same mode. This can cause the dead section to rupture. If a person is not provided with urgent medical care, then the risk of death is high.
Heart rhythm disorder
It is provoked by a spasmodic artery or untimely impulses that arose against the background of impaired conduction of the coronary vessels.
The main symptoms of manifestation:
- Sensation of tremors in the region of the heart;
- A sharp fading of contractions of the heart muscle;
- dizziness, blurriness, darkness in the eyes;
- The severity of breathing;
- Unusual manifestation of passivity (in children);
- Lethargy in the body, constant fatigue;
- Pressing and prolonged (sometimes sharp) pain in the heart.
Rhythm failure often manifests itself due to a slowdown in metabolic processes if the endocrine system is out of order. It can also be a catalyst for long-term use of many drugs.
This concept is the definition of insufficient activity of the heart, which is why there is a shortage of blood supply to the whole organism.
Pathology can develop as a chronic complication of arrhythmia, heart attack, weakening of the heart muscle.
Acute manifestation is most often associated with the intake of toxic substances, injuries and a sharp deterioration in the course of other heart diseases.
This condition needs urgent treatment, otherwise the likelihood of death is high.
 Against the background of diseases of the coronary vessels, the development of heart failure is often diagnosed.
Against the background of diseases of the coronary vessels, the development of heart failure is often diagnosed. The main symptoms of manifestation:
- Violation of the heart rhythm;
- Difficulty breathing;
- Coughing fits;
- Blurring and darkening in the eyes;
- Swelling of the veins in the neck;
- Swelling of the legs, accompanied by painful sensations;
- Disconnection of consciousness;
- Strong fatigue.
Often this condition is accompanied by ascites (accumulation of water in the abdominal cavity) and an enlarged liver. If a patient has persistent hypertension or diabetes mellitus, it is impossible to make a diagnosis.
coronary insufficiency
Heart failure is the most common type of ischemic disease. It is diagnosed if the circulatory system has partially or completely stopped supplying blood to the coronary arteries.
The main symptoms of manifestation:
- Severe pain in the region of the heart;
- Feeling of "lack of space" in the chest;
- Discoloration of urine and its increased excretion;
- Paleness of the skin, a change in its shade;
- The severity of the work of the lungs;
- Sialorrhoea (intense salivation);
- Nausea, vomiting, rejection of the usual food.
In the acute form, the disease is manifested by an attack of sudden cardiac hypoxia due to arterial spasm. Chronic course is possible due to angina pectoris against the background of accumulation of atherosclerotic plaques.
There are three stages in the course of the disease:
- Initial (mild);
- Expressed;
- A severe stage that, if not properly treated, can lead to death.
Causes of vascular problems
There are several factors contributing to the development of CHD. Many of them are a manifestation of insufficient care for one's health.
Important! Today, according to medical statistics, cardiovascular diseases are the number 1 cause of death in the world.
 Every year, more than two million people die from coronary artery disease, most of whom are part of the population of "prosperous" countries, with a comfortable sedentary lifestyle.
Every year, more than two million people die from coronary artery disease, most of whom are part of the population of "prosperous" countries, with a comfortable sedentary lifestyle. The main causes of ischemic disease can be considered:
- Tobacco smoking, incl. passive inhalation of smoke;
- Eating foods high in cholesterol
- Excess weight (obesity);
- Hypodynamia, as a consequence of a systematic lack of movement;
- Exceeding the norm of sugar in the blood;
- Frequent nervous tension;
- Arterial hypertension.
There are also factors independent of a person that affect the state of blood vessels: age, heredity and gender.
Women are more resistant to such ailments and therefore they are characterized by a long course of the disease. And men more often suffer precisely from the acute form of pathologies that end in death. Surgical intervention is prescribed in case of ineffectiveness of traditional therapy. To better nourish the myocardium, coronary bypass surgery is used - they connect the coronary and external veins where the intact portion of the vessels is located. Dilation can be performed if the disease is associated with hyperproduction of the artery wall layer. This intervention involves the introduction of a special balloon into the lumen of the vessel, expanding it in places of a thickened or damaged shell.
Heart before and after chamber dilatation
Reducing the risk of complications
Own preventive measures reduce the risk of coronary artery disease. They also minimize the negative consequences during the rehabilitation period after treatment or surgery.
The simplest advice available to everyone:
- Rejection of bad habits;
- Balanced diet (special attention to Mg and K);
- Daily walks in the fresh air;
- Physical activity;
- Control of blood sugar and cholesterol;
- Hardening and sound sleep.
The coronary system is a very complex mechanism that needs to be treated with care. The pathology that has manifested once is steadily progressing, accumulating more and more new symptoms and worsening the quality of life, therefore, the recommendations of specialists and the observance of elementary health standards should not be neglected.
Systematic strengthening of the cardiovascular system will allow you to keep the vigor of the body and soul for many years.
Video. Angina. Myocardial infarction. Heart failure. How to protect your heart.
Anatomy of the coronary circulation highly variable. Features of the coronary circulation of each person are unique, like fingerprints, therefore, each myocardial infarction is "individual". The depth and prevalence of a heart attack depend on the interweaving of many factors, in particular, on the congenital anatomical features of the coronary bed, the degree of development of collaterals, the severity of atherosclerotic lesions, the presence of "prodromes" in the form of angina, which first occurred during the days preceding the infarction (ischemic "training" of the myocardium), spontaneous or iatrogenic reperfusion, etc.
As is known, heart receives blood from two coronary (coronary) arteries: the right coronary artery and the left coronary artery [respectively a. coronaria sinistra and left coronary artery (LCA)]. These are the first branches of the aorta that depart from its right and left sinuses.
Barrel LKA[in English - left main coronary artery (LMCA)] departs from the upper part of the left aortic sinus and goes behind the pulmonary trunk. The diameter of the LCA trunk is from 3 to 6 mm, the length is up to 10 mm. Usually the trunk of the LCA is divided into two branches: the anterior interventricular branch (AMV) and the circumflex (Fig. 4.11). In 1/3 of cases, the LCA trunk is divided not into two, but into three vessels: the anterior interventricular, circumflex, and median (intermediate) branches. In this case, the median branch (ramus medianus) is located between the anterior interventricular and envelope branches of the LCA.
This vessel- analogue of the first diagonal branch (see below) and usually supplies the anterolateral sections of the left ventricle.
Anterior interventricular (descending) branch of the LCA follows the anterior interventricular sulcus (sulcus interventricularis anterior) towards the apex of the heart. In English literature, this vessel is called the left anterior descending artery: left anterior descending artery (LAD). We will adhere to the more accurate anatomically (F. H. Netter, 1987) and the term "anterior interventricular branch" accepted in the domestic literature (O. V. Fedotov et al., 1985; S. S. Mikhailov, 1987). At the same time, when describing coronarograms, it is better to use the term "anterior interventricular artery" to simplify the name of its branches.
main branches latest- septal (penetrating, septal) and diagonal. The septal branches depart from the PMA at a right angle and deepen into the thickness of the interventricular septum, where they anastomose with similar branches extending from below the posterior interventricular branch of the right coronary artery (RCA). These branches may differ in number, length, direction. Sometimes there is a large first septal branch (going either vertically or horizontally - as if parallel to the PMA), from which branches extend to the septum. Note that of all areas of the heart, the interventricular septum of the heart has the densest vascular network. The diagonal branches of the PMA run along the anterolateral surface of the heart, which they supply with blood. There are from one to three such branches.
In 3/4 cases of PMV does not end in the region of the apex, but, bending around the latter on the right, wraps itself on the diaphragmatic surface of the posterior wall of the left ventricle, supplying both the apex and partially the posterior diaphragmatic sections of the left ventricle, respectively. This explains the appearance of the Q wave on the ECG in lead aVF in a patient with extensive anterior infarction. In other cases, ending at the level or not reaching the apex of the heart, PMA does not play a significant role in its blood supply. Then the apex receives blood from the posterior interventricular branch of the RCA.
proximal area front The interventricular branch (PMV) of the LCA is called the segment from the mouth of this branch to the origin of the first septal (penetrating, septal) branch or to the origin of the first diagonal branch (less stringent criterion). Accordingly, the middle section is a segment of the PMA from the end of the proximal section to the departure of the second or third diagonal branch. Next is the distal section of the PMA. When there is only one diagonal branch, the boundaries of the middle and distal sections are approximately defined.
Educational video of the blood supply of the heart (anatomy of arteries and veins)
In case of problems with viewing, download the video from the pagecoronary arteries stomach and heart. - B. arteries of the stomach(arteriae coronariae ventriculi) depart from the celiac artery (art. coeliaca) or its branches (hepatic artery, splenic, etc.). There are four of them; of these, two are connected at the lesser curvature of the stomach and thus form the upper arterial arch of the stomach (arcus arteriosus ventriculi superior); the other two, merging at the greater curvature, form the lower arterial arch of the stomach. A mass of small branches depart from both arterial arches, which enter the wall of the stomach and here break up into the smallest blood stems. B. artery heart (arteria coronaria cordis) - a branch that gives the main vascular trunk of the body (see Aorta), while still in the cavity of the pericardial sac. Starting with two openings lying approximately at the same height as the free edge of the aortic semilunar valves, two V. arteries depart from the expanded part of the latter, called the bulb, and go to the anterior surface of the heart, to its transverse groove. Here, both V. arteries diverge: the right one goes to the right edge of the heart, bends around it, passes to the back surface and along the posterior longitudinal groove reaches the apex of the heart, into the tissue of which it enters; the left gives first a large branch, reaching along the anterior longitudinal groove to the apex of the heart, then goes to the left edge of the heart, passes to the back and here, at the height of the transverse groove, enters the muscles of the heart. Throughout its length, both V. arteries give small branches that penetrate into the thickness of the wall of the heart. The right V. artery supplies blood to the walls of the right atrium, the right ventricle, the apex of the heart, and, in part, the left ventricle; left - apex of the heart, left atrium, left ventricle, ventricular septum. If an animal artificially closes or even only narrows the lumen of the V. artery, then after a while the heart stops contracting (cardiac paralysis), since the heart muscle can work correctly only as long as the V. arteries supply it with sufficient blood necessary for nourishment. quantity. On V. arteries of the human heart, there are pathological changes that affect in a similar way, that is, they completely stop or significantly reduce the flow of blood to the walls of the heart (see Arteriosclerosis, Thrombosis, Embolism) and thereby entail instant death or very painful suffering - myocarditis with its consequences (aneurysm, rupture, heart attack), often angina pectoris, and so on.
Encyclopedic Dictionary F.A. Brockhaus and I.A. Efron. - St. Petersburg: Brockhaus-Efron. 1890-1907 .
See what "Coronary arteries" are in other dictionaries:
Trunk arteries - … Atlas of human anatomy
- (Greek, singular artēría), blood vessels that carry oxygenated (arterial) blood from the heart to all organs and tissues of the body (only the pulmonary artery carries venous blood from the heart to the lungs). * * * ARTERIES ARTERIES (Greek, singular… … encyclopedic Dictionary
Arteries that supply blood to the heart muscle. The right and left coronary arteries (right and left coronary arteries) depart from the bulb and give off branches that supply the heart. See Coronary angioplasty. Bypass vascular shunt. Source:… … medical terms
CORONARY ARTERIES, CORONARY ARTERIES- (coronary arteries) arteries supplying blood to the heart muscle. The right and left coronary arteries (right and left coronary arteries) depart from the bulb and give off branches that supply the heart. See Coronary angioplasty. Bypass shunt ... ... Explanatory Dictionary of Medicine
Vessels of the heart- Arteries. The blood supply to the heart is carried out by two arteries: the right coronary artery, a. coronaria dextra, and the left coronary artery, a. coronaria sinistra, which are the first branches of the aorta. Each of the coronary arteries comes out of ... ... Atlas of human anatomy
HEART- HEART. Contents: I. Comparative anatomy........... 162 II. Anatomy and histology ........... 167 III. Comparative physiology .......... 183 IV. Physiology .................. 188 V. Pathophysiology ................. 207 VI. Physiology, pat. ... ...
ANGINA PECTORIS- Angina pectoris, (angina pectoris, synonymous with Heberden's asthma), in its essence, is primarily a subjective syndrome, manifesting itself in the form of severe retrosternal pain, accompanied by a sense of fear and a sense of the immediate proximity of death. Story. 21… Big Medical Encyclopedia
In the diagram, the Aorta (lat..arteria ortha, a.ortha direct artery [source not specified 356 days]) is the largest unpaired arterial vessel of the great circle ... Wikipedia
LICHTENBERG- Alexander (Alexander Lich tenberg, born in 1880), an outstanding contemporary German. urologist. He was an assistant to Czerny and Narath. In 1924, he received the head of the urological department in the Catholic church of St. Hedwigs in Berlin, to a swarm in ... ... Big Medical Encyclopedia
The science that studies the structure of the body, individual organs, tissues and their relationships in the body. All living things are characterized by four features: growth, metabolism, irritability and the ability to reproduce themselves. The combination of these signs ... ... Collier Encyclopedia